0B1. 引言
近年来,随着胃肠道肿瘤发病率的增加,其受到越来越多的重视。胃丛状纤维黏液瘤(plexiform fibromyxoma, PF)是一种临床罕见的胃间质性肿瘤,从2007年Takahashi等人首次报道至今,文献中仅报道了130余病例。临床工作中容易误诊为胃肠道间质瘤(Gastrointestinal stromal tumor, GIST)。本文报道了1例胃窦部丛状纤维黏液瘤,并对其临床、病理及影像学表现进行了文献复习,以期提高临床对PF的认识。
1B2. 病例资料
患者女性,20岁,3天前无明显诱因出现呕血伴黑便,黑便2次,呕吐物为胃内容物及黑色物质,伴心慌、头晕,无反酸、烧心等。
电子胃镜显示:胃窦黏膜充血水肿,红白相间,以红为主,前壁可见一巨大黏膜下隆起,大小约5 × 7 cm,表面破溃,可见血栓头。胃镜检查诊断:胃粘膜下隆起,间质瘤可能大。见图1。
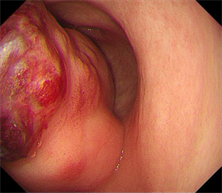
Figure 1. Electronic gastroscopy showed the surface of huge submucosal eminence in the anterior wall of gastric antrum was broken
图1. 电子胃镜示胃窦前壁巨大黏膜下隆起,表面破溃
全腹CT平扫 + 强化显示:胃窦前壁团块状软组织肿块,最大截面约6.6 × 3.6 cm,形态不规则,其内密度不均,增强扫描呈不均匀渐进性明显强化,黏膜线局部不连续,胃窦部壁外见增粗迂曲血管影。
手术记录:术中见肿瘤位于胃窦近幽门,约5 × 5 cm,腔外生长。区域淋巴结见明显肿大。打开肌层,见肿瘤沿肌层间隙生长,与周围有明显界限,沿肌层游离肿瘤,至肿瘤根部,提起距肿瘤蒂根部约3 cm处,以派尔特腔内闭合器,离断切除肿瘤及部分正常胃壁。见图2。
病理:(胃窦)丛状纤维黏液瘤
免疫组化结果:CD117(−),Dog-1(−),CD34 (血管+),S-100(−),SMA(+),Desmin (少量+),SDHB(+),Ki67-MIB1 (2%),CD10 (灶+)见图3。

Figure 2. (A) CT plain scan (B) CT arterial phase (C) CT venous phase (D) CT delayed phase. The anterior wall mass of gastric antrum was irregular in shape and uneven in density, and the enhanced scan showed uneven gradual obvious enhancement
图2. (A) CT平扫 (B) CT动脉期 (C) CT静脉期 (D) CT延迟期。胃窦前壁肿块,形态不规则,内密度不均,增强扫描呈不均匀渐进性明显强化

Figure 3. HE staining and immunohistochemical staining
图3. HE染色及免疫组化染色
2B3. 讨论
3.1. 命名
胃丛状血管黏液肌纤维母细胞瘤(plexiform angiomyxoid myofibroblastic tumor, PAMT),是2007年由Takahashi等人 [1] 首次报道的一种罕见的胃间质肿瘤。在2009年,Miettinen等人 [2] 认为用丛状纤维黏液瘤(plexiform fibromyxoma, PF)一词更能表明其组织学形态。2010年WHO消化系统肿瘤分类在胃间质肿瘤这一分类中,也采用了丛状纤维黏液瘤这一命名。尽管WHO分类中使用了“丛状纤维黏液瘤”这一命名,但许多作者仍然认为“丛状血管黏液肌纤维母细胞瘤”一词更能描述此类肿瘤的组织发生和组织学特征,因此,在文献中“丛状血管黏液肌纤维母细胞瘤”和“丛状纤维黏液瘤”均被用来命名该病。
3.2. 临床特征
迄今为止,文献中仅发表了130余病例 [3]。Miettinen [2] 及Su [4] 等人认为胃PF的发病率非常低,不到胃肠道间质瘤(GIST)的1/150。患者年龄范围很广,从5岁到81岁(平均年龄为43.17岁 ± 18.00岁;中位年龄为46岁)均可发病。患者多为中老年人,发病高峰期通常在30~60岁之间,女性略多于男性 [4]。临床表现 [4] 主要分为一般胃肠道症状(如腹痛、腹胀、消化不良、食欲不振、烧心、腹泻和上腹部不适等)和消化道出血症状 [5] (如贫血、黑便和呕血等),也可因肿瘤破裂出现急腹症 [3]。有部分病例是体检发现 [6]。
病变通常位于胃窦(占79%) [4] [7],但偶尔也可位于胃的其他部位 [6] [8]、小肠 [9] [10]、大肠、纵隔 [11] 和食道等 [4]。根据最近的一份文献报告,肿瘤的最大直径范围为0.8~17 cm,平均大小为4.81 ± 3.30 cm,中位大小为4.0 cm [4]。
5B3.3. 病理
PF主要起源于黏膜下层和固有肌层,可以向黏膜及浆膜层蔓延,引起溃疡和/或穿孔。肉眼观,表现为分叶状浅粉色、棕白色或灰白色肿块,切口表面呈凝胶状、囊状,伴有黏液,多结节或息肉状生长,无包膜,边缘清楚(但有时不清楚),常可见出血 [4] [12]。镜下观,肿瘤组织主要由多发黏液样结节组成,被固有纤维或平滑肌组织所包绕,边缘可呈浸润性,结节直径约0.1~0.7 cm,为卵圆形或短梭形细胞散在分布于黏液样或纤维黏液样基质中,通常有典型的分支状毛细血管网,局部间质胶原化可较明显。未见肿瘤坏死和钙化。肿瘤细胞胞质不明显,胞界不清,核呈卵圆形,染色质尘状,核仁细小,细胞异质性小,核分裂活性低,周围有边界不清晰的轻度嗜酸性粒细胞质。
特殊染色:黏液样基质阿辛蓝染色阳性,PAS染色阳性。免疫组化染色:Vimentin,SMA,MAS呈阳性,表明PF的成纤维细胞,肌成纤维细胞和平滑肌细胞特征。目前的研究报告表明,Vimentin、SMA和MSA对PF的诊断具有较高的敏感性和特异性,主要是因为它们是平滑肌肿瘤和间质组织的重要标志物。CD10、Caldesmon、Desmin可以为阳性,提示可能存在的肌纤维母细胞分化。Desmin和Caldesmon是肌肉谱系走向终末肌肉细胞分化的更特异性标志物,并且在PF中表现出有限和局灶性反应结果,与PF细胞发育的肌成纤维细胞谱系一致。CD34、CK、S-100、CD117、DOG-1、ALK-1、β连接素均阴性,表明PF是一种不同于GIST、血管黏液瘤、神经源性肿瘤、肉瘤样癌和炎性肌纤维母细胞瘤的疾病实体。CD34大多为阴性(95.1%),但在几个病例中显示了局部阳性结果,CD34可以在具有成纤维细胞性质的细胞中被标记,在血管内皮组织中显示强阳性染色,因此,局灶性阳性的结果可能由于PF的丰富血管造成的。S100蛋白可以在胃肠道的梭形细胞肿瘤中表达,这是神经鞘瘤的特征。CD117或DOG1在PF中通常为阴性,但在GIST中为阳性,因此,它可以用于GIST与PF的鉴别。一些病例报告显示,标本对PR呈局灶性或弥漫性阳性,但对ER呈阴性。因此,激素治疗也是一个需要考虑的方向,但它可能意义不大。Ki-67非常低,大多 < 2% [1] [2] [4] [12] - [17]。
一些研究也研究了基因突变。C-KIT和PDGFRA基因突变在 GIST 中具有重要的特性 [18],但在报告的所有PF病例中均呈阴性,从而进一步证实了PF和GIST之间存在区别。一些病例描述存在t(11; 12) (q11; q13)染色体易位,形成MALAT1-GLI1基因融合,通过GLI1过表达或GLI1上调,造成了部分肿瘤的发生 [4] [13] [17] [19] [20]。
6B3.4. 影像学表现
对于胃PF,CT及MRI检查是术前常用的无创检查,其对于定位、分期及制定手术计划来说至关重要。遗憾的是,文献记载的影像学检查比较少。CT上主要表现为边界清楚,实性/囊性/囊实性的肿块 [21],增强扫描实性部分动脉期轻度增强,静脉期及延迟期强化程度进一步增加 [16] [22] [23] [24] [25],囊性成分没有明显增强 [26]。既往文献中,进行MRI检查的病例相对少见,胃PF在T1WI加权像上表现为低信号,在T2WI加权像上表现为高信号,DWI未见明显弥散受限,在增强扫描时,实性部分也表现出不均匀渐进性明显强化 [9] [26] [27] [28]。渐进性强化的模式与PF的黏液样基质的特征相符合。大部分病灶实性部分明显强化 [6] [29],可能与其内含丰富血管有关;部分文献报道肿块整体为轻度强化 [30],但他们文献中的图像是动脉期图像,轻度强化的原因可能与扫描时间太早无法准确反映黏液成分的强化有关。需要注意的是,仅仅通过影像学准确诊断PF还是有一定的难度。
7B3.5. 治疗及预后
PF的主要治疗方法是手术切除 [31],部分胃切除术和远端胃切除术是PF最常用的手术方式,其次是局部切除术、胃次全切除术等。内镜下切除术相对少见 [13]。所有手术治疗的病例均未出现严重的术后并发症 [4]。
PF以前多被认为是一种良性疾病,随访的病例中未发现复发及转移 [4] [21]。然而,Miettinen等人 [2] 和Kawara [32] 等人报告了血管和淋巴侵犯,最近Ayyanar等人 [33] 报告了一例经内镜黏膜下剥离术后一年复发及远处转移的病例,这提示我们是否将PF定义为良性肿瘤,仍需要更多的病例进行论证。
8B3.6. 鉴别诊断
PF的鉴别诊断包括以下内容:1) GIST:GIST是胃肠道中最常见的间质肿瘤,也是PF最重要的鉴别诊断,许多PF患者最初被误诊为GIST。从影像学上,GIST好发于胃底和胃体大弯侧,体积小时边界清晰,密度均匀;大于5 cm时常伴有出血、坏死及囊变,可以是实性/囊实性/囊性,强化方式多种多样,仅通过影像学难以与PF鉴别,Yang等人 [26] 认为GIST常见的囊性表现包括单房或多房厚壁囊实性肿块,增强为边缘强化 [34],而PF为边界清楚的腔外囊实性肿块,增强为渐进性不均匀强化。从病理上,黏液样GIST可以显示丛状或多结节生长模式,包括丰富的黏液样基质和梭形细胞增殖,类似于PF,但是,肿瘤细胞对CD117,C-KIT,DOG-1和CD34呈阳性,C-KIT或PDGFRA突变的基因检测可以将它们与PF区分开来 [18] [24] [35]。2) 胃肠道神经鞘瘤:是一种比较罕见的胃肠道肿瘤。在影像学上,CT多为低密度,密度均匀,很少囊变坏死 [36],这与其他部位的神经鞘瘤很不一样,周围可有反应性淋巴结增生,增强扫描呈延迟强化,强化程度多为轻–中度强化。在病理上,部分神经鞘瘤可显示丛状生长的模式 [35],但免疫组化测定显示S100阳性,DOG-1和C-KIT阴性,SRY相关的HMGbox 10阳性 [16] [37]。3) 胃平滑肌瘤:真正的胃平滑肌瘤很少见。在影像学上,多是位于贲门附近向腔内生长的肿块,少见钙化及坏死,增强扫描多为轻度均匀强化 [36]。在病理上,SMA、MSA、desmin和caldesmon在平滑肌瘤中呈阳性 [5]。
综上所述,PF临床相对少见,其发病机制及遗传学等需要进一步研究,其典型影像学表现能与病理一一对应,但临床容易误诊为GIST。作为影像科医生,当发现胃窦部肿块,黏膜下及肌层生长为主,增强扫描渐进性明显强化时,应考虑到本病的可能。
15B参考文献
[1] Takahashi, Y., Shimizu, S., Toida, S., et al. (2007) Plexiform Angiomyxoid Myofibroblastic Tumor of the Stomach. The American Journal of Surgical Pathology, 31, 724-728. https://doi.org/10.1097/01.pas.0000213448.54643.2f
[2] Miettinen, M., Makhlouf, H.R., Sobin, L.H., et al. (2009) Plexiform Fibromyxoma: A Distinctive Benign Gastric Antral Neoplasm Not to Be Confused with a Myxoid Gist. American Journal of Surgical Pathology, 33, 1624-1632. https://doi.org/10.1097/PAS.0b013e3181ae666a
[3] Zhang, R., Xia, L.-G., Huang, K.-B., et al. (2022) Huge Gastric Plexiform Fibromyxoma Presenting as Pyemia by Rupture of Tumor: A Case Report. World Journal of Clinical Cases, 10, 2253-2260. https://doi.org/10.12998/wjcc.v10.i7.2253
[4] Su, H.-A., Yen, H.-H. and Chen, C.-J. (2019) An Update on Clinicopathological and Molecular Features of Plexiform Fibromyxoma. Canadian Journal of Gastroenterology and Hepatology, 2019, Article ID: 3960920. https://doi.org/10.1155/2019/3960920
[5] Mustafa, T., Suarez, Y. and Damani, T. (2021) Plexiform Angiomyxoid Myofibroblastic Tumor (PAMT) of the Stomach: An Extremely Rare Mesenchymal Tumor Masquerading as Gastrointestinal Stromal Tumor or Leiomyoma. Journal of Gastrointestinal Surgery, 25, 3265-3267. https://doi.org/10.1007/s11605-021-05069-z
[6] Kang, Y., Jung, W., Do, I.-G., et al. (2012) Plexiform Angiomyxoid Myofibroblastic Tumor of the Stomach: Report of Two Cases and Review of the Literature. Korean Journal of Pathology, 46, 292-296. https://doi.org/10.4132/KoreanJPathol.2012.46.3.292
[7] Li, X., Li, S., Xiong, S., et al. (2018) A Rare Case of Plexiform Angiomyxoid Myofibroblastic Tumor in the Stomach Which Was Diagnosed at the Earliest Stage in the Literature. Gastroenterology Report, 6, 313-316. https://doi.org/10.1093/gastro/gow035
[8] Ebi, M., Nagao, K., Sugiyama, T., et al. (2022) Gastric Plexiform Fibromyxoma Resected Using Nonexposed Endoscopic Wall-Inversion Surgery: A Case Report. Case Reports in Gastroenterology, 16, 159-164. https://doi.org/10.1159/000522411
[9] Lu, S. and Guo, L. (2022) Duodenal Plexiform Fibromyxoma: A Case Report. Asian Journal of Surgery, 45, 2554-2555. https://doi.org/10.1016/j.asjsur.2022.05.150
[10] Zhang, W.-G., Xu, L.-B., Xiang, Y.-N., et al. (2018) Plexiform Fibromyxoma of the Small Bowel: A Case Report. World Journal of Clinical Cases, 6, 1067-1072. https://doi.org/10.12998/wjcc.v6.i15.1067
[11] Duckworth, L.V., Gonzalez, R.S., Martelli, M., et al. (2014) Plexiform Fibromyxoma: Report of Two Pediatric Cases and Review of the Literature. Pediatric and Developmental Pathology, 17, 21-27. https://doi.org/10.2350/13-09-1373-OA.1
[12] 王凤华, 陈峥嵘, 牛会林, 等. 胃丛状纤维黏液瘤: 一种独特的胃窦良性肿瘤[J]. 中华病理学杂志, 2012, 41(3): 190-191.
[13] Wu, J.-D., Chen, Y.-X., Luo, C., et al. (2021) Plexiform Angiomyxoid Myofibroblastic Tumor Treated by Endoscopic Submucosal Dissection: A Case Report and Review of the Literature. World Journal of Gastroenterology, 27, 5288-5296. https://doi.org/10.3748/wjg.v27.i31.5288
[14] 胡桂明, 陈慧萍, 刘秋雨, 等. 胃丛状纤维黏液瘤临床病理学分析[J]. 中华病理学杂志, 2018, 47(4): 258-262.
[15] 魏建国, 刘文英, 孙爱静. 胃丛状纤维黏液瘤一例[J]. 中华病理学杂志, 2015, 44(1): 61-62.
[16] Ma, S., Wang, J., Lu, Z., et al. (2021) Plexiform Fibromyxoma: A Clinicopathological and Immunohistochemical Analysis of Two Cases with a Literature Review. Journal of International Medical Research, 49. https://doi.org/10.1177/03000605211027878
[17] 闫红燕, 王晓敏, 陈红芳, 等. 胃丛状血管黏液样肌纤维母细胞瘤临床病理特点与预后分析[J]. 现代肿瘤医学, 2022, 30(9): 1617-1620.
[18] Miettinen, M. and Lasota, J. (2013) Gastrointestinal Stromal Tumors. Gastroenterology Clinics of North America, 42, 399-415. https://doi.org/10.1016/j.gtc.2013.01.001
[19] Spans, L., Fletcher, C.D., Antonescu, C.R., et al. (2016) Recurrent MALAT1-GLI1 Oncogenic Fusion and GLI1 Up-Regulation Define a Subset of Plexiform Fibromyxoma. The Journal of Pathology, 239, 335-343. https://doi.org/10.1002/path.4730
[20] Li, J., Gao, H., Lv, M., et al. (2019) Gastric Plexiform Fibromyxoma: A Rare Case in a 5-Year-Old Male. Pediatric Blood & Cancer, 66, e27638. https://doi.org/10.1002/pbc.27638
[21] Perry, L., Mccann, C., Schwartz, J., et al. (2020) Plexiform Angiomyxoid Myofibroblastic Tumor of the Stomach. The American Surgeon, 89, 145-146. https://doi.org/10.1177/0003134820951487
[22] Arslan, M.E., Li, H., Fu, Z., et al. (2021) Plexiform Fibromyxoma: Review of Rare Mesenchymal Gastric Neoplasm and Its Differential Diagnosis. World Journal of Gastrointestinal Oncology, 13, 409-423. https://doi.org/10.4251/wjgo.v13.i5.409
[23] Nagahisa, Y., Itou, T., Okita, C., et al. (2016) Laparoscopic and Endoscopic Cooperative Surgery for Plexiform Angiomyxoid Myofibroblastic Tumor. Case Reports in Gastroenterology, 10, 302-307. https://doi.org/10.1159/000446764
[24] Hu, G., Chen, H., Liu, Q., et al. (2017) Plexiform Fibromyxoma of the Stomach: A Clinicopathological Study of 10 Cases. International Journal of Clinical and Experimental Pathology, 10, 10926-10933.
[25] 潘馨梦, 张梦梅, 杨亚英, 等. 胃丛状纤维黏液瘤1例[J]. 中国医学影像技术, 2021, 37(3): 453. https://doi.org/10.13929/j.issn.1003-3289.2021.03.033
[26] Yang, M.-X., Zhao, Z.-H., Yang, J.-F., et al. (2017) Imaging Findings of Gastric Plexiform Fibromyxoma with a Cystic Change: A Case Report and Review of Literature. Medicine, 96, e8967. https://doi.org/10.1097/MD.0000000000008967
[27] Akai, H., Kiryu, S., Shinozaki, M., et al. (2017) Computed Tomography and Magnetic Resonance Imaging of a Plexiform Angiomyxoid Myofibroblastic Tumor: A Case Report. BMC Medical Imaging, 17, 7. https://doi.org/10.1186/s12880-017-0180-1
[28] Sakamoto, K., Hirakawa, M., Atsumi, K., et al. (2014) A Case of Gastric Plexiform Fibromyxoma: Radiological and Pathological Findings. Japanese Journal of Radiology, 32, 431-436. https://doi.org/10.1007/s11604-014-0315-z
[29] Jonaitis, L., Kiudelis, M., Slepavicius, P., et al. (2016) Plexiform Angiomyxoid Myofibroblastic Tumor of Stomach: A Rare Case. World Journal of Gastrointestinal Endoscopy, 8, 674-678. https://doi.org/10.4253/wjge.v8.i18.674
[30] Sing, Y., Subrayan, S., Mqadi, B., et al. (2010) Gastric Plexiform Angiomyxoid Myofibroblastic Tumor: Gastric Plexiform Angiomyxoid Tumor. Pathology International, 60, 621-625. https://doi.org/10.1111/j.1440-1827.2010.02569.x
[31] Banerjee, S., De La Torre, J., Burgoyne, A.M., et al. (2019) Gastric Plexiform Fibromyxoma. Journal of Gastrointestinal Surgery, 23, 1936-1939. https://doi.org/10.1007/s11605-019-04132-0
[32] Kawara, F., Tanaka, S., Yamasaki, T., et al. (2017) Gastric Plexiform Fibromyxoma Resected by Endoscopic Submucosal Dissection after Observation of Chronological Changes: A Case Report. World Journal of Gastrointestinal Oncology, 9, 263-267. https://doi.org/10.4251/wjgo.v9.i6.263
[33] Ayyanar, P., Nayak, H.K., Samal, S.C., et al. (2022) Recurrent Plexiform Angiomyxoid Myofibroblastic Tumour (PAMT) of the Stomach with Aggressive Behaviour. Pathology, 54, 650-654. https://doi.org/10.1016/j.pathol.2021.09.010
[34] Lee, J., Park, C.M., Kim, K.A., et al. (2010) Cystic Lesions of the Gastrointestinal Tract: Multimodality Imaging with Pathologic Correlations. Korean Journal of Radiology, 11, 457-468. https://doi.org/10.3348/kjr.2010.11.4.457
[35] Li, B., Zhang, Q.-F., Han, Y.-N., et al. (2015) Plexiform Myxoid Gastrointestinal Stromal Tumor: A Potential Diagnostic Pitfall in Pathological Findings. International Journal of Clinical and Experimental Pathology, 8, 13613-13618.
[36] Kang, H.C., Menias, C.O., Gaballah, A.H., et al. (2013) Beyond the Gist: Mesenchymal Tumors of the Stomach. Radiographics, 33, 1673-1690. https://doi.org/10.1148/rg.336135507
[37] Voltaggio, L., Murray, R., Lasota, J., et al. (2012) Gastric Schwannoma: A Clinicopathologic Study of 51 Cases and Critical Review of the Literature. Human Pathology, 43, 650-659. https://doi.org/10.1016/j.humpath.2011.07.006
NOTES
*第一作者。
#通讯作者。