摘要: 目的:探讨血清血管内皮生长因子(VEGF)、人附睾蛋白4 (HE4)、糖类抗原125 (CA125)、糖类抗原724 (CA724)在卵巢恶性肿瘤中的诊断价值。方法:回顾性分析郑州大学人民医院2020至2021年的卵巢恶性肿瘤患者106例,按术后常规病理结果将其分为上皮性肿瘤组97例、生殖细胞肿瘤组5例、性索间质肿瘤组4例。测定各组患者血清VEGF、HE4、CA125、CA724水平,绘制受试者工作特征(ROC)曲线并计算曲线下面积(AUC),计算各血清标志物的敏感性和特异性,比较单项及联合检测对卵巢恶性肿瘤的诊断价值。结果:ROC曲线显示在上皮性卵巢癌与非上皮性卵巢癌的鉴别诊断及FIGO分期的鉴别诊断中,血清VEGF、HE4、CA125、CA724的4项指标的联合检测的AUC明显高于单项检测、2项及3项指标的联合检测,且敏感度和特异性更高,差异有统计学意义(P < 0.05)。结论:血清VEGF、HE4、CA125及CA724的水平与卵巢恶性肿瘤的发生发展密切相关,可作为卵巢恶性肿瘤鉴别诊断的检测指标,且联合检测诊断效能更高,对卵巢恶性肿瘤的早期诊断具有重要意义。
Abstract:
Objective: To investigate the diagnostic value of serum vascular endothelial growth factor (VEGF), human epididymis protein 4 (HE4), carbohydrate antigen 125 (CA125), and carbohydrate antigen 724 (CA724) in ovarian malignant tumors. Methods: 106 patients with ovarian malignant tumors in the People’s Hospital of Zhengzhou University from 2020 to 2021 were retrospectively analyzed. According to the postoperative routine pathological results, they were divided into 97 cases of epi-thelial tumors, 5 cases of germ cell tumors, and 4 cases of sex cord-stromal tumors. The levels of VEGF, HE4, CA125, and CA724 in the serum of patients in each group were measured, the ROC curve of subjects was drawn, the area under the curve (AUC) was calculated, and the sensitivity and speci-ficity of serum markers were calculated, and the diagnostic value of single and combined detection for ovarian malignant tumors was compared. Results: The ROC curve showed that in the differential diagnosis of epithelial ovarian cancer and non-epithelial ovarian cancer and the differential diagno-sis of FIGO staging, the AUC of the combined detection of serum VEGF, HE4, CA125, CA724 was sig-nificantly higher than that of the single detection, the combined detection of two and three indica-tors, and the sensitivity and specificity were higher, with a statistically significant difference (P < 0.05). Conclusion: The levels of VEGF, HE4, CA125, and CA724 in serum are closely related to the occurrence and development of ovarian malignant tumors, which can be used as the detection indi-cators for differential diagnosis of ovarian malignant tumors, and the combined detection has high-er diagnostic efficacy, which is of great significance for the early diagnosis of ovarian malignant tu-mors.
1. 引言
癌症是世界范围内的一个主要公共健康问题,据世界卫生组织发布的数据显示,2020年我国新发癌症人数和癌症死亡人数,均位居全球首位,已成为威胁人们健康和生命的头号杀手 [1]。其中卵巢癌是妇科肿瘤中恶性程度最高的癌症,发病率仅次于宫颈癌和子宫内膜癌,其高死亡率和发病率使其严重影响到女性的身体健康和生活质量 [2]。卵巢癌可分为两个主要的组织学亚型:上皮性卵巢癌(Epithelial ovarian cancer, EOC),约占卵巢癌的90%,以及非上皮性卵巢癌(Non-Epithelial ovarian cancer, NEOC),约占卵巢癌的10% [3]。EOC又包括浆液性癌(高级别浆液性癌和低级别浆液性癌)、黏液性癌、子宫内膜样癌和透明细胞癌 [4] [5]。早期卵巢癌患者症状及体征不明显且缺乏有效的筛查手段,超过70%的患者确诊时已为晚期 [6] [7]。目前,晚期EOC的标准治疗方法是肿瘤细胞减灭术结合铂类和紫杉醇化疗 [8],以及靶向治疗 [9] 或免疫抑制剂治疗 [10]。这些治疗手段虽然提高了EOC近期的治疗结果,但由于药物剂量限制性毒性和卵巢癌多药耐药(Multidrug resistance, MDR)的出现,严重影响了药物疗效 [11],即使积极治疗后EOC依然有70%~80%的复发率,且癌细胞腹腔广泛的种植转移致使转移率能够达到40%~62%,预后较差 [12]。因此为了提高卵巢癌患者的生存率,改善患者预后,急需新的灵敏度高、特异性强的早期筛查方式。目前,随着分子生物学的快速发展和实验室检测技术的不断进步,越来越多的分子肿瘤标记物被发现与卵巢癌的生物学行为密切相关。
CA125是目前临床诊断卵巢癌最常用的经典标志物,尤其是诊断EOC的首选标志物,在监测卵巢癌病情和预后方面也有重要价值 [13]。血清CA125在卵巢癌的早期筛查中意义重大,但单独的检测并不足以满足早期筛查的需求,需要寻找其他指标或者方法学进行联合分析。目前,新的血清肿瘤标记物,包括VEGF,HE4和CA724已经被提出并评估,有研究表明,VEGF是一种具有重要促血管生成活性的生长因子,积极参与调节正常和病理性血管生成过程,是肿瘤发展的关键因素 [14]。HE4是近年来发现的一种新的卵巢癌相关肿瘤标记物,在早期卵巢癌诊断中具有重要潜力 [15]。CA724水平在包括卵巢癌在内的各种上皮癌中升高 [16],因此有可以成为卵巢癌诊断的检测指标。
因此,我们评估了血清VEGF、HE4、CA125和CA724在卵巢恶性肿瘤中的诊断效能,研究上述肿瘤标记物联合检测对于提高良恶性肿瘤诊断率的能力,并探讨其与卵巢恶性肿瘤病理类型及临床分期的相关性,旨在为构建预测癌症的风险模型提供依据。
2. 资料与方法
2.1. 研究对象
回顾性分析2021年1月至10月在郑州大学人民医院诊治的106例卵巢恶性肿瘤患者,纳入标准:年龄 > 18岁;于我院完成初次手术,未在手术前进行化疗药物治疗;病理科确诊;血清学检查资料无缺失。排除标准:非原发肿瘤或合并其他肿瘤;临床信息不全及随访失联;不能耐受手术或中途转院;妊娠期妇女。该106例卵巢恶性肿瘤患者年龄14~81岁,中位年龄为55 (53.70 ± 13.40)岁。从病理组织学划分,卵巢恶性肿瘤组分为上皮性卵巢癌97例,非上皮性卵巢癌9例,见表1。根据FIGO发布的标准,将该106例恶性肿瘤组进行临床分期,I~II期30例,III~IV期96例。
2.2. 研究方法
各组患者在术前诊断时,清晨抽取患者空腹外静脉血5 mL,3000 r/min离心5~10分钟,分离出上清液,利用电化学发光法测定血清CA125 (0~6.9 U/mL)及CA724 (0~6.9 U/mL)水平;使用酶联免疫吸附试验测定血清VEGF (0~160 pg/mL)及HE4 (0~140 pmol/L)水平。
2.3. 统计方法
采用SPSS 21.0统计学软件、MedcCalc软件和GraphPad Prism 8.3.0软件分析数据,计量资料用均数 ± 标准差(
)表示,组间比较采用两独立样本t检验;计数资料采用χ2检验。利用受试者工作特征(Receiver Operator Characteristic, ROC)曲线,采用二元逻辑回归分析计算单项和联合指标检测因素模型,计算曲线下面积(AUC)和95%置信区间(95% CI)。以P < 0.05为差异有统计学意义。
3. 结果
3.1. 患者临床特征
纳入研究的106例卵巢恶性肿瘤患者中,上皮性卵巢癌96例(90.57%)最常见,其中以浆液性囊腺癌74例(69.81%)最多见。见表1。其中该卵巢恶性肿瘤患者中处于I~II期的30例(28.30%),III~IV期的76例(71.70%),提示大多数恶性肿瘤在FIGO III~IV期时被诊断。

Table 1. Pathological types of ovarian malignant tumors (n = 106)
表1. 卵巢恶性肿瘤病理学类型(n = 106)
3.2. 血清VEGF、HE4、CA125及CA724在卵巢癌不同病理类型中的ROC曲线分析
单项指标中,CA125的诊断效能较高,AUC为0.911 (95% CI: 0.839, 0.957),敏感度和特异性分别为83.51%和100%。2项联合指标中,VEGF + CA125的AUC最大,为0.923 (95% CI: 0.830, 0.974),敏感度和特异性分别为86.44%和100.00%。3项联合指标中,VEGF + HE4 + CA125的AUC最大,为0.924 (95% CI: 0.830, 0.975),敏感度和特异性分别为86.21%和100%。4项联合指标中,VEGF + HE4 + CA125 + CA724的AUC为0.938 (95% CI: 0.861, 0.986),敏感度和特异性分别为88.82%和100%。差异均具有统计学意义(P < 0.05)。见图1及表2。
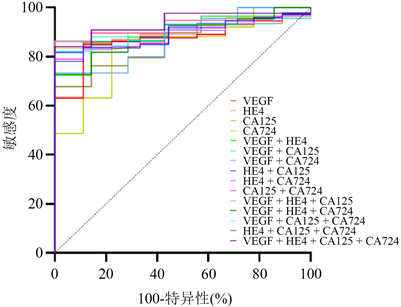
Figure 1. ROC curve of EOC and NEOC in differentiation of ovarian cancer by serum tumor markers
图1. 血清肿瘤标志物鉴别卵巢癌EOC与NEOC的ROC曲线

Table 2. Diagnostic value of single and combined detection of serum tumor markers for different pathological types of ovarian cancer
表2. 血清肿瘤标志物单项及联合检测对卵巢癌不同病理类型的诊断价值
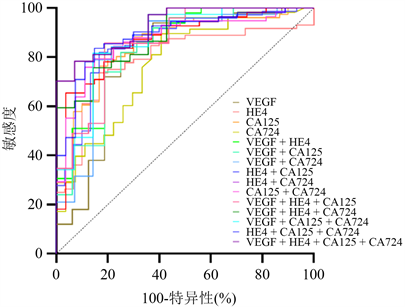
Figure 2. ROC curve of serum tumor markers in differentiating ovarian cancer stage I~II from stage III~IV
图2. 血清肿瘤标志物在鉴别卵巢癌I~II期与III~IV期的ROC曲线

Table 3. Diagnostic value of single and combined detection of serum tumor markers in FIGO staging of ovarian cancer
表3. 血清肿瘤标志物单项及联合检测对卵巢癌FIGO分期的诊断价值
3.3. 血清VEGF、HE4、CA125及CA724在卵巢癌FIGO I~II期与III~IV期中的ROC曲线分析
单项指标中,HE4的诊断效能较高,AUC为0.861 (95% CI: 0.779, 0.922),敏感度和特异性分别为80.56%和83.33%。2项联合指标中,HE4 + CA125的AUC最大,为0.880 (95% CI: 0.790, 0.942),敏感度和特异性分别为74.55%和88.59%。3项联合指标中,VEGF + HE4 + CA125的AUC最大为0.918 (95% CI: 0.820, 0.982),敏感度和特异性分别为100%和83.43%。4项联合指标中,VEGF + HE4 + CA125 + CA724的AUC最大,0.921 (95% CI: 0.847, 0.989),敏感度和特异性分别为100%和89.43%。差异均具有统计学意义(P < 0.05)。见图2及表3。
4. 讨论
肿瘤分子标志物是肿瘤细胞分泌的或细胞癌变过程中肿瘤与宿主相互作用产生的物质,它们的发生或数量的变化反映了肿瘤的存在和生长。正常组织和良性病变组织中几乎不产生或甚至不产生肿瘤分子标志物,这些分子标志物存在于肿瘤细胞和组织中,也可以进入血液或其他体液,并且随着肿瘤的发展和进展,含量会显著增加。此外,它们数量的变化可用于早期诊断和评估恶性肿瘤的生物学行为,如临床分期、复发和转移 [17]。血清肿瘤标志物检测具有采集方便、创伤小、简便准确、成本低等优点,是目前恶性肿瘤早期诊断的主要手段。血清学筛查可为早期卵巢癌筛查提供参考,尤其是可为早期EOC筛查提供实验室依据,从而指导早期EOC的诊断和治疗 [18]。
CA125是一种重要的广谱糖蛋白指标,癌细胞膜表面相关糖蛋白的分解代谢促进CA125的表达,其表达的变化表明癌细胞具有持续性扩散的风险 [19]。HE4因在卵巢癌细胞上高表达,可促进卵巢生发上皮细胞的持续增殖和分化受损,从而干扰癌细胞粘附和侵袭的病理过程 [20]。VEGF对内皮细胞具有促有丝分裂和抗凋亡作用,增加血管通透性,促进细胞迁移等,在肿瘤血管生成和血管系统的维持中起到重要作用 [14]。CA724是一种糖蛋白,在包括胃癌、乳腺癌和卵巢腺癌等各种上皮性癌症患者的血清中升高 [16]。虽然CA724不如CA125敏感,但不受月经周期或妊娠的影响 [21]。血清VEGF、HE4、CA125、CA724均在在卵巢癌的诊断方面有一定的检测价值,但单项检测指标的灵敏度及特异性较低。
ROC曲线是敏感度和特异性的综合,以评价特定指标的诊断效能和寻找最佳的诊断标志物。因此为了优化卵巢癌早期诊断和评估治疗的效果,本研究分析了VEGF、HE4、CA125、CA724在卵巢肿瘤诊断中的ROC曲线,并比较其特异性、敏感度和AUC,以分析上述指标在卵巢恶性肿瘤分型及分期鉴别诊断中的诊断效能。根据ROC曲线的AUC大小,VEGF、HE4、CA125、CA724单项指标及联合指标在EOC与NEOC诊断价值方面,VEGF + HE4 + CA125 + CA724联合检测的诊断价值更好(AUC = 0.938),敏感度88.82%,特异性100%,优于单项检测、2项联合检测和3项联合检测。对上述血清标志物在卵巢癌分期的诊断价值进行分析发现,VEGF + HE4 + CA125 + CA724联合检测的诊断价值更好(AUC = 0.921),敏感度100%,特异性89.43%,同样优于单项检测、2项联合检测和3项联合检测。从上述结果来看,单项标志物的检测不够灵敏和准确,与单项检测相比,VEGF + HE4 + CA125 + CA724联合检测的漏诊率降低,准确率提高,尤其是在卵巢癌的早期诊断方面,4项联合检测更具有诊断价值。
综上所述,利用ROC曲线分析,血清肿瘤分子标记物VEGF、HE4、CA125及CA724在卵巢癌的病理类型及FIGO分期上的表达存在差异,且联合检测指标较单项检测提高了卵巢癌诊断的灵敏度、特异性,具有更好的诊断效能,对卵巢恶性肿瘤的早期诊断具有重要意义。
基金项目
2020年河南省重点研发与推广专项,编号:212102310042。
声明
相关数据已获得病人知情同意和伦理批准。
NOTES
*通讯作者。