1. 引言
多囊卵巢综合征(Polycystic Ovary Syndrome, PCOS)是以月经异常、多毛、痤疮、卵巢多囊样改变及糖、脂代谢紊乱为主要特征的生殖内分泌代谢性疾病。高尿酸血症(Hyperuricemia, HUA)是指机体尿酸生成过多和/或排泄减少,导致血清尿酸水平升高的一种病理状态。PCOS患者高尿酸血症的患病率约为正常女性的3倍 [1] 。尿酸水平升高可能增加PCOS患者发生糖脂代谢异常的风险 [2] [3] 。因此,PCOS患者尿酸水平可能反映其糖脂代谢状况。
目前临床上常采用口服葡萄糖耐量试验(Oral Glucose Tolerance Test, OGTT)及口服葡萄糖胰岛素释放试验(Oral Glucose Insulin Releasing Test, OGIRT)来评估PCOS患者的糖代谢异常,但部分患者对多次采血操作产生抗拒,依从性低,且整个采血过程耗时长,检测成本较高。如尿酸水平能用于PCOS患者糖代谢异常的初步筛查,将有助于减轻患者的生理和心理负担,节约时间和经济成本。因尿酸检测费用远低于血脂,将其用于PCOS患者脂代谢异常的初步筛查,也能降低患者的经济成本。
Oda等 [4] 在2559例患者中发现尿酸是筛查健康人群发生代谢综合征的独立预测因子;巩伟伟 [5] 等报道HUA组非酒精性脂肪性肝病患者发生心脑血管事件概率达22.91%;Zoppini G等 [6] 研究发现194例HUA患者发生糖尿病肾病概率为29.5%。血清尿酸水平与空腹血糖、餐后2 h血糖、稳态模型胰岛素抵抗指数(Homeostatic Model Assessment of Insulin Resistance, HOMA-IR)、甘油三酯和低密度脂蛋白水平之间存在正相关 [7] 。因此,血清尿酸有望成为PCOS患者糖脂代谢异常的初筛指标。本研究旨在评估PCOS患者血清高尿酸水平与糖、脂代谢异常的相关性,探讨血清尿酸初步筛查PCOS患者糖、脂代谢异常的临床价值。
2. 对象与方法
2.1. 研究对象
本回顾性研究连续纳入2022年1月~2023年9月于重庆医科大学附属第二医院妇产科就诊的PCOS患者124例。根据我院实验室参考值,高尿酸血症定义为血清尿酸 ≥ 360 μmol/L。血清尿酸水平 ≥ 360 μmol/L定义为HUA组,血清尿酸水平 < 360 μmol/L定义为正常组。PCOS的诊断根据2003年鹿特丹标准 [8] 。纳入标准:年龄18~45岁。排除标准:1) 近3月服用可能影响血糖、血脂、血清尿酸水平的药物;2) 继发性高尿酸血症:糖原累积病Ⅰ型,Lesch Nyhan综合征、白血病、多发性骨髓瘤、淋巴瘤等疾病导致及恶性肿瘤化疗和放疗后发生的血清尿酸水平升高;3) 慢性肾脏病患者因肾小管分泌尿酸减少而使血清尿酸水平增高。本研究经医院医学伦理委员会审批通过。
2.2. 观察指标
1) 性激素指标:黄体生成素(LH)、卵泡刺激素(FSH)、雌二醇(E2)、孕酮(P)、泌乳素(PRL)、睾酮(T)、硫酸脱氢表雄酮(DHEA-S)、性激素结合球蛋白(SHBG),游离雄激素指数(FAI);2) 年龄、身高、体重、腰围(WC)、臀围(HC);计算体重指数(BMI)、腰臀比(WHR);3) 糖代谢指标:空腹血糖(FPG)、OGTT 2 h血糖(2hPG)、空腹胰岛素(FINS);4) 脂代谢指标:总胆固醇(TC)、甘油三酯(TG)、高密度脂蛋白胆固醇(HDL-c)、低密度脂蛋白胆固醇(LDL-c);5) 血清尿酸。
2.3. 糖、脂代谢异常的定义
1) 糖代谢异常:空腹血糖 ≥ 7.0 mmol/L或OGTT 2 h血糖 ≥ 11.1 mmol/L为糖尿病;糖调节受损(IGR)包括糖耐量异常(IGT)和空腹血糖受损(IFG):OGTT 2 h血糖 ≥ 7.8 mmol/L且<11.1 mmol/L为IGT,空腹血糖 ≥ 6.1 mmol/L且<7 mmol/L为IFG;HOMA-IR ≥ 2.69判定为胰岛素抵抗 [9] ;2) 脂代谢异常根据我院实验室参考值定义:TC ≥ 5.18 mmol/L和(或) TG ≥ 1.70 mmol/L和(或) LDL-c ≥ 3.37 mmol/L和(或) HDL-c ≤ 1.29 mmo/L。
2.4. 统计学方法
计量资料采用Shapiro-Wilk检验对其进行正态性检验,符合正态分布的计量资料以平均值 ± 标准差表示,组间比较采用t检验;非正态分布的计量资料使用中位数和四分位数表示,组间比较采用Mann-Whitney U检验。计数资料采用例数及百分比表示,组间比较采用χ2检验。先采用单因素Logistic回归分析筛选可能影响PCOS患者糖、脂代谢异常的因素,将P ≤ 0.20的因素纳入多因素Logistic回归,筛选影响PCOS患者糖、脂代谢异常的独立危险因素。绘制血清尿酸筛查PCOS患者糖、脂代谢异常的受试者工作特征曲线(Receiver Operating Characteristic Curve, ROC)。使用混淆矩阵评价糖、脂代谢异常的分类准确程度。采用SPSS26.0软件对研究数据进行统计分析,P < 0.05为差异有统计学意义。
3. 结果
3.1. 基线资料比较
本研究共纳入124例PCOS患者,其中高尿酸血症患者47例,占比37.9%。研究结果显示,HUA组体重、WC、HC、BMI、WHR、T、FAI均呈显著增加(P < 0.05);HUA组SHBG水平较正常组降低(P < 0.05);年龄、身高、LH、FSH、E2、P、PRL、DHEA-S在两组间的差异无统计学意义(P > 0.05)。见表1。

Table 1. Baseline characteristics of the subjects
表1. 研究对象的基线特征
3.2. 糖、脂代谢指标比较
HUA组FINS、HOMA-IR、2hPG、TG均呈显著增加(P < 0.05);HUA组HDL-c水平较正常组降低(P < 0.05);FPG、TC、LDL-c在两组间的差异无统计学意义(P > 0.05)。见表2。

Table 2. Comparison of metabolic indexes of glucose and lipid
表2. 糖、脂代谢指标比较
3.3. HUA组与正常组的糖、脂代谢异常率比较
HUA组糖代谢异常率(70.2% vs. 35.1%, P = 0.000)、胰岛素抵抗率(65.96% vs. 27.27%, P = 0.000)和脂代谢异常率(82.98% vs. 53.25%, P = 0.001)较正常组显著增高。见表3。

Table 3. Comparison of abnormal rates of glucose and lipid metabolism between the HUA group and normal group
表3. HUA组与正常组糖、脂代谢异常率的比较
3.4. 影响PCOS患者糖、脂代谢异常的相关性分析
3.4.1. PCOS患者糖、脂代谢异常的单因素Logistic回归分析
应用单因素Logistic回归分析对可能影响PCOS患者糖、脂代谢异常的混杂因素进行筛选,将P ≤ 0.20的因素,即可能影响PCOS患者糖、脂代谢异常的因素作为多因素Logistic回归的协变量进行分析。研究发现,HUA是PCOS患者糖代谢异常(OR = 1.341, 95% CI 1.125~9.928, P = 0.035)和脂代谢异常(OR = 3.835, 95% CI 1.245~11.809, P = 0.019)发生的危险因素。见表4、表5。

Table 4. Univariate Logistic regression analysis of abnormal glucose metabolism
表4. 糖代谢异常的单因素Logistic回归分析

Table 5. Univariate Logistic regression analysis of abnormal lipid metabolism
表5. 脂代谢异常的单因素Logistic回归分析
3.4.2. PCOS患者糖、脂代谢异常的多因素Logistic回归分析
HUA是PCOS患者发生糖代谢异常(OR = 3.406, 95% CI 1.414~8.207, P = 0.006)和脂代谢异常(OR = 3.321, 95% CI 1.231~8.963, P = 0.018)的独立危险因素。见表6、表7。

Table 6. Multivariate analysis of abnormal glucose metabolism by Logistic regression analysis
表6. 糖代谢异常的多因素分析Logistic回归分析

Table 7. Multivariate analysis of abnormal lipid metabolism by Logistic regression analysis
表7. 脂代谢异常的多因素分析Logistic回归分析
3.5. 血清尿酸筛查PCOS患者糖、脂代谢异常的ROC曲线分析
血清尿酸筛查PCOS患者糖、脂代谢异常的曲线下面积分别为0.652、0.709,临界筛查值分别为340.9 μmol/L、320.5 μmol/L,灵敏度分别为60.00%、73.80%,特异度分别为76.60%、68.20%。结果显示,血清尿酸对PCOS患者糖、脂代谢异常均具有一定的筛查价值,见图1、图2。
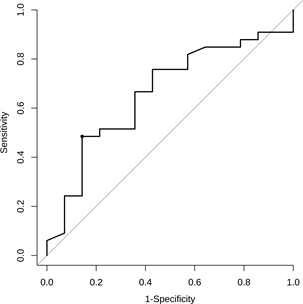
Figure 1. ROC curve analysis of serum uric acid screening for abnormal glucose metabolism
图1. 血清尿酸筛查糖代谢异常的ROC曲线分析
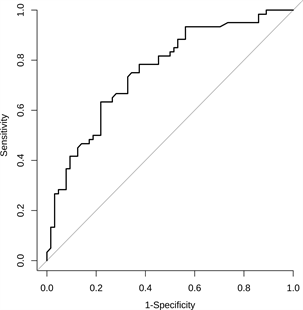
Figure 2. ROC curve analysis of serum uric acid screening for abnormal lipid metabolism
图2. 血清尿酸筛查脂代谢异常的ROC曲线分析
3.6. 糖、脂代谢异常初筛结果
血清尿酸对糖、脂代谢异常初筛正确的PCOS患者例数分别为101例、109例,脂代谢异常初筛正确的PCOS患者例数略高于糖代谢异常初筛正确患者例数。见表8、表9。

Table 8. Results of preliminary screening classification of abnormal glucose metabolism
表8. 糖代谢异常初筛分类结果
(注:1代表糖代谢异常;0代表糖代谢正常)。

Table 9. Results of preliminary screening classification of abnormal lipid metabolism
表9. 脂代谢异常初筛分类结果
(注:1代表脂代谢异常;0代表脂代谢正常)。
3.7. 糖、脂代谢异常初筛性能评价
糖、脂代谢异常初筛的分类准确率分别为81.45%、87.90%,精确率分别为78.46%、90.12%,召回率分别为85.00%、91.25%。血清尿酸对PCOS患者糖、脂代谢异常的初筛性能较好。见表10。

Table 10. Evaluation of primary screening performance of abnormal glucose and lipid metabolism
表10. 糖、脂代异常初筛性能评价
(注:准确率是指所有筛查正确样本占总样本的比重;精确率是指在筛查代谢异常的样本中,筛查正确的比重;召回率是指在实际代谢异常的样本中,筛查正确的比重)。
4. 讨论
本研究通过对PCOS患者HUA组及正常组的糖、脂代谢数据进行分析,探讨血清尿酸能否初步筛查PCOS患者的糖、脂代谢异常。研究结果表明,HUA组糖、脂代谢异常率较正常组显著增高;多因素Logistic回归分析显示,血清高尿酸水平是PCOS患者糖、脂代谢异常的独立危险因素;ROC曲线提示,血清尿酸对PCOS患者糖、脂代谢异常均具有一定的筛查价值;初筛性能评价显示,血清尿酸对糖、脂代谢异常的初筛性能较好。
我们的研究发现HUA组的胰岛素抵抗率较正常组显著增高。Qiu等 [10] 发现PCOS患者尿酸水平和HOMA-IR值呈正相关。Kawai [11] 等提出HUA可能是胰岛素抵抗的独立预测因子。前述研究提示HUA可能导致PCOS患者胰岛素抵抗的发生。HUA导致胰岛素抵抗的机制可能有以下几方面:一氧化氮是辅助胰岛素促进组织细胞摄取利用葡萄糖的重要分子 [12] ,尿酸可与一氧化氮直接反应生成不稳定的亚硝化尿酸产物,从而降低机体内源性一氧化氮的合成介导胰岛素抵抗,其分子机制可能在于一氧化氮介导的成骨骼肌细胞及脂肪细胞的胰岛素受体/胰岛素受体底物1/磷脂酰肌醇-3-激酶/蛋白激酶B/内皮型一氧化氮合酶转导通路受损 [13] ,最终致血糖摄取下降。HUA通过刺激机体产生炎症反应,分泌大量炎性因子,干扰胰岛素介导的脂肪细胞和肝脏对葡萄糖的吸收,从而降低胰岛素生物学效应,诱发胰岛素抵抗 [14] ;此外,血清尿酸水平持续升高可使尿酸盐结晶沉积在胰岛β细胞,导致胰岛β细胞功能受损,从而引起糖代谢异常 [15] 。
HUA组患者脂代谢异常率及甘油三酯水平明显高于正常组,且HUA组高密度脂蛋白胆固醇水平较正常组降低。Gil-Campos等 [16] 发现血清尿酸与甘油三酯水平呈正相关。Liu等 [17] 报道,在PCOS患者中,高尿酸水平者的血脂水平明显高于正常者。以上研究提示HUA可能引起PCOS患者血脂异常。HUA可能会减少甘油三酯分解代谢酶的数量或降低其活性,从而导致血中甘油三酯水平的升高 [18] 。同时,HUA可加强磷酸戊糖代谢途径,增加还原型烟酰胺腺嘌呤二核苷酸磷酸的产生,进而促进脂肪合成增加,引起血甘油三酯水平升高 [19] ,最终导致PCOS患者脂代谢异常的发生。初筛性能评价结果显示,血清尿酸水平筛查PCOS患者糖、脂代谢异常的分类准确率分别为81.45%、87.90%,精确率分别为78.46%、90.12%,召回率分别为85.00%、91.25%,提示糖、脂代谢异常的漏诊率低,尿酸用于筛查PCOS患者糖、脂代谢异常的性能较好。在我院门诊实验室检查中,PCOS诊疗过程涉及的OGTT和OGIRT检验费合计252.00元,血脂检验费为69.30元,而尿酸的检验费为10.50元。采用检测尿酸水平初筛PCOS患者糖、脂代谢异常,可大幅度减少患者的经济负担,并能避免OGTT和OGIRT多次采血对患者造成的心理压力,缩短患者就诊时间。
在本研究中,由于样本量小,且为回顾性研究,存在一定局限性,未来的研究需扩大样本量、采用前瞻性研究验证血清尿酸对PCOS患者糖、脂代谢异常的筛查价值。
综上,PCOS患者血清尿酸水平与糖脂代谢异常密切相关,血清尿酸水平筛查PCOS患者糖、脂代谢异常的性能较好,有望成为初筛指标,未来将开展前瞻性验证性研究来进一步评价血清尿酸水平筛查PCOS患者糖、脂代谢异常的临床价值。
NOTES
*第一作者。
#通讯作者。