摘要: 目的:本实验拟制备一种具有优越的机械性、自愈性、粘附性、光热转化性和细胞相容性的智能纳米复合水凝胶,以增强伤口愈合过程。方法:首先通过柠檬酸钠还原法制备金纳米颗粒(AuNPs)溶液。接着,通过离心法获得富血小板血浆(PRP),将碳化钛(Ti
3C
2)和金纳米颗粒(AuNPs)引入到血小板水凝胶中,最终获得了金纳米/聚丙烯酰胺/碳化钛/富血小板血浆(
AuNPs/PAM/Ti
3C
2/PRP)水凝胶。对水凝胶进行表征,证明其成功制备,并进一步研究其促进皮肤创面愈合的作用。结果:AuNPs/PAM/Ti
3C
2/PRP水凝胶呈疏松多孔状、孔径均一。且水凝胶具有良好的光热转化作用。体外实验证明AuNPs/PAM/Ti
3C
2/PRP水凝胶对细胞无明显毒害作用,而且还能促进细胞的增殖和迁移。结论:成功构建了具有拉伸性、自愈性、粘附性、光热转化性和细胞相容性的AuNPs/PAM/Ti
3C
2/PRP智能复合纳米水凝胶,其展现出良好的促细胞增殖和迁移的作用,在治疗皮肤损伤上具有很大的应用前景,有望成为新型伤口敷料。
Abstract:
Objective: In this experiment, it is proposed to prepare a smart nanocomposite hydrogel with superior mechanical, self-healing, adhesion, photothermal conversion and cytocompatibility to enhance the wound healing process. Methods: Firstly, gold nanoparticles (AuNPs) solution was prepared by sodium citrate reduction method. Then, platelet-rich plasma (PRP) was obtained by centrifugation, and titanium carbide (Ti3C2) and gold nanoparticles (AuNPs) were introduced into the platelet hydrogel, and finally the gold nano/polyacrylamide/titanium carbide/platelet-rich plasma (AuNPs/PAM/Ti3C2/PRP) hydrogel was obtained. The hydrogels were characterized to demonstrate their successful preparation and further investigated for their role in promoting skin wound healing. Results: The AuNPs/PAM/Ti3C2/PRP hydrogels were loose and porous with uniform pore size. And the hydrogel has a good photothermal conversion effect. In vitro experiments demonstrated that AuNPs/PAM/Ti3C2/PRP hydrogels had no obvious toxic effects on cells and also promoted cell proliferation and migration. Conclusion: AuNPs/PAM/Ti3C2/PRP smart composite nanohydrogels with stretchability, self-healing, adhesion, photothermal conversion and cytocompatibility were successfully constructed, which exhibited good pro-cell proliferation and migration, and have great application prospects in the treatment of skin injuries, and are expected to become a new type of wound dressing.
1. 引言
皮肤是覆盖于人体表面的最大的器官,具有高度自我修复和更新的能力,在机体防御中起着至关重要的作用。机体因手术或意外受到创伤时会造成皮肤完整性破坏,使其防御能力受损,尤其是较大损伤如全层皮肤损伤很难恢复皮肤的原始生物学特性 [1] 。创面修复缓慢甚至停止的原因主要有以下几种:1) 创面发生感染或有坏死组织存在 [2] ;2) 创面局部皮肤温度偏低 [3] ;3) 创面局部生长因子浓度和活性过低或缺乏生长因子 [4] ;4) 修复细胞结构异常和凋亡 [5] 。
传统的治疗方法包括清创、外科手术和纱布覆盖等,但这些治疗方法很难达到一个好的治疗效果。近来随着伤口敷料的不断更新,伤口敷料已经从包覆型敷料发展到具有促伤口愈合功能的敷料。理想的伤口敷料应具备优异的组织相容性、适宜的保湿能力 [6] 、足够的机械强度 [7] 等。碳化钛(Ti3C2)作为一种新兴的二维纳米材料,具有良好的生物相容性,且在具有优异的光热转化能力,在光热治疗(PTT)上具有巨大的应用潜力 [8] ,被认为是理想的光热转化材料 [9] 。富血小板血浆是新鲜抗凝全血经过两次离心法获得的,其含有高浓度血小板 [10] 。除血小板外,PRP还含有大量的生长因子,如血管内皮生长因子(VEGF)、转化生长因子-β (TGF-β)、表皮生长因子(EGF)、胰岛素样生长因子(IGF)和P血小板源性生长因子(PDGF)等 [11] [12] ,这些生长因子能够减轻炎症反应,促进血管生成,促进成纤维细胞和表皮细胞等生长,同时加速新老细胞的更替。
在本实验中,将碳化钛、金纳米颗粒溶液引入到血小板凝胶中,制备了一种具有优异可拉伸性和粘附性、良好生物相容性和光热转化性能的金纳米/聚丙烯酰胺/碳化钛/富血小板血浆(AuNPs/PAM/Ti3C2/PRP)纳米复合水凝胶。并验证其表征和促细胞增殖和迁移能力,为皮肤伤口修复提供新的思路。
2. 实验方法
2.1. 实验材料
N,N'-双(丙烯酰)胱胺,上海麦克林生化科技有限公司;丙烯酰胺,上海麦克林生化科技有限公司;CCK-8试剂盒,MedChemExpress;Calcein/PI双染试剂盒,上海碧云天生物技术有限公司;DMEM培养基,胎牛血清(FBS),美国GIBCO公司。
2.2. AuNPs/PAM/Ti3C2/PRP纳米复合水凝胶的制备
首先,制备金纳米颗粒溶液 [13] ,将100 mL 0.3 mmol/L氯金酸(HAuCl4)放入油浴锅中磁性搅拌,使其升温至100℃后,继续搅拌5~10 min,后在沸腾的氯金酸(HAuCl4)溶液中加入2 mL 38.7 mmol/L柠檬酸钠溶液,继续加热至烧瓶中的溶液由黄色转变为酒红色后,停止加热,将反应后的溶液静置待其冷却,即获得所需的纳米颗粒形貌的金纳米颗粒材料分散液。
然后,制备AuNPs/PAM/Ti3C2水凝胶溶液,向5 mL金纳米颗粒溶液中依次加入1000 mg AM单体,6 mg·N,N'-双(丙稀酰)胱胺和15 mg KPS,然后进行超声溶解,使其形成均匀分散的AuNPs/PAM/Ti3C2水凝胶溶液。
最后,制备AuNPs/PAM/Ti3C2/PRP纳米复合水凝胶,本次实验中所用富血小板血浆(Platelet-Rich Plasma, PRP)是由血小板通过离心法制备,其中血小板的浓度为1500~2000 × 1011/L。向AuNPs/PAM/Ti3C2水凝胶溶液中分别加入50% PRP并彻底混合(前期已通过预实验确定水凝胶与PRP的最适成胶比例),后加入引发助剂四甲基乙二胺(TMEDA) 10 uL静置成胶。
2.3. AuNPs/PAM/Ti3C2/PRP纳米复合水凝胶的表征
2.3.1. 扫描电子显微镜(SEM)
将冻干后的凝胶样品置于制样盘中并用导电胶进行固定,然后置于喷金机中进行喷金处理,后即可使用扫描电子显微镜表征AuNPs/PAM/Ti3C2/PRP水凝胶和AuNPs/PAM/Ti3C2/PRP水凝胶的形貌。
2.3.2. AuNPs/PAM/Ti3C2/PRP水凝胶粘附性测试
将AuNPs/PAM/Ti3C2/PRP水凝胶样品分别将其与人体腕关节、橡胶等材料表面进行粘附测试。
2.3.3. AuNPs/PAM/Ti3C2/PRP水凝胶拉伸性测试
将AuNPs/PAM/Ti3C2/PRP纳米复合水凝胶用模具制备成圆柱形进行拉伸测试。
2.3.4. AuNPs/PAM/Ti3C2/PRP水凝胶体外光热转化性能研究
将AuNPs/PAM/Ti3C2、AuNPs/PAM/Ti3C2/PRP水凝胶及PBS置于激光器下,使激光光源与水凝胶的距离为8~10 cm,用激光器808 nm不同功率(0.25、0.4、0.75、1 W/cm2)照射8 min,通过红外成像仪观察水凝胶表面温度的变化。
2.3.5. AuNPs/PAM/Ti3C2/PRP水凝胶自愈性测试
将完整的水凝胶从中间切割,然后将其切面重新合在一起,再用NIR (808 nm 1 W/cm2)照射。后用镊子夹起照射后的水凝胶并向相反方向拉扯,观察切口的愈合情况。
2.4. 细胞实验
2.4.1. 细胞培养
小鼠成纤维细胞(L929)由青岛大学附属医院西海岸院区中心实验室提供。使用含有90% DMEM基础培养基、1%青霉素/链霉素双抗溶液和10% FBS的完全培养基对细胞进行培养,后置入37℃、含5%二氧化碳的恒温细胞培养箱(WCI-180N)中孵育。待细胞融合度达80%时进行传代,在细胞传代中,胰酶起到消化细胞的作用。传代过程中多余细胞使用细胞冻存液置于液氮中保存。
2.4.2. 体外生物相容性研究
为了研究AuNPs/PAM/Ti3C2/PRP纳米复合材料的细胞相容性,首先将L929细胞进行复苏、传代培养,取对数生长期的细胞,以6 × 104个/mL的浓度接种于96孔板上,并用培养基孵育过夜,使细胞贴壁。实验组加入AuNPs/PAM/Ti3C2和AuNPs/PAM/Ti3C2/PRP水凝胶浸提液孵育24 h (以0.1 g/mL比例进行浸提),每个浓度设5个复孔,对照组加细胞悬液和DMEM,空白组加DMEM。孵育结束后,使用CCK-8试剂盒检测L929细胞相对存活率。
将L929细胞以6 × 104/孔的密度接种于96孔板中,完全培养基孵育过夜,使细胞贴壁。后使用Calcein/PI双染试剂盒进行细胞染色,活细胞被染成绿色,死细胞被染成红色。置于荧光显微镜下观察细胞存活和死亡情况,进一步评估水凝胶的细胞相容性。每组设五个复孔,重复三次实验。
2.5. 统计学分析
使用SPSS26.0软件进行统计学分析。定量资料以均数 ± 标准差(Means ± SD)表示,两组间均数数比较采用两独立样本t检验(independent samples t-test),P < 0.05认为差异具有统计学意义。
3. 结果与讨论
3.1. AuNPs/PAM/Ti3C2/PRP水凝胶的表征
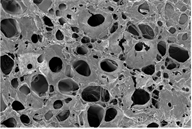
通过扫描电子显微镜显示了水凝胶的三维网络。图1(a)和图1(b)显示,AuNPs/PAM/Ti3C2和AuNPs/PAM/Ti3C2/PRP水凝胶均呈现出明显的多孔网络结构,且多孔之间呈现良好的连通性。这种多孔网络结构有利于水凝胶对伤口渗出液的吸收,同时有效促进营养物质的传送和代谢废物的运输,促进细胞更好地生长。
 (a)
(a) 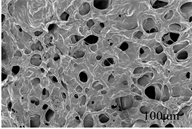 (b)
(b)
Figure 1. The SEM images of AuNPs/PAM/Ti3C2 hydrogel (a) and AuNPs/PAM/Ti3C2/PRP hydrogel (b)
图1. AuNPs/PAM/Ti3C2水凝胶(a)和AuNPs/PAM/Ti3C2/PRP水凝胶(b)的扫描电子显微镜(SEM)图像
3.2. AuNPs/PAM/Ti3C2/PRP水凝胶的粘附性和拉伸性评价
水凝胶具有优异的粘附性能,能够满足水凝胶敷料的粘合剂要求 [14] 。如图2(a)所示,AuNPs/PAM/Ti3C2/PRP水凝胶表现出较好的粘附力,能够牢固的粘贴在人体腕关节和橡胶上。用于伤口敷料的水凝胶材料不仅应具备良好的粘附性,还要具有优异的弹性,能够牢固粘附在不平整创面和关节伤口上而不随着人体运动导致水凝胶破裂甚至脱落。如图2(b)所示,本实验所设计的AuNPs/PAM/Ti3C2/PRP智能纳米复合水凝胶通过金–硫动态配位作用拥有强大的拉伸性能,可以拉伸数倍,满足了不平整创面及关节处伤口对敷料反复拉伸和粘附的要求。

Figure 2. Adhesion (a) and tensile properties tests (b) of the hydrogel
图2. 水凝胶的粘附(a)和拉伸性能测试(b)
3.3. AuNPs/PAM/Ti3C2/PRP水凝胶的光热转化性能研究
由于AuNPs表面等离子体的共振效应,其在400~700 nm范围内有很强的吸收峰,具有显著的光热转换能力;Ti3C2在近红外区域具有高光热转化效率。用波长为808 nm、功率为0.4 W∙cm−2的激光分别照射PBS溶液、AuNPs/PAM/Ti3C2水凝胶和AuNPs/PAM/Ti3C2/PRP水凝胶溶液。如图3(a)所示,作为对照的PBS在激光照射下温度变化不大,仅能达到36.5℃,而AuNPs/PAM/Ti3C2水凝胶和AuNPs/PAM/Ti3C2/PRP水凝胶在激光照射下,凝胶表面温度逐渐升高。在照射8 min后,温度分别上升到为40.5℃和41.0℃。证明水凝胶纳米复合材料具有优异的光热升温性能。且功率越大,水凝胶的光热效应越强(图3(b))。有研究表明温度过高会损伤正常组织,当温度在40℃~41℃时,能够促进血管新生和内皮细胞形成。这为水凝胶联合光热治疗促进皮肤修复提供了理论支撑。
 (a)
(a)  (b)
(b)
Figure 3. (a) Heating effect of PBS, AuNPs/PAM/Ti3C2 hydrogel and AuNPs/PAM/Ti3C2/PRP hydrogel irradiated by NIR (808 nm, 0.4 W∙cm−2) for 8 min. (b) Heating effect of AuNPs/PAM/Ti3C2/PRP hydrogel irradiated by NIR (808 nm) with different powers (0.25, 0.4, 0.75, 1 W∙cm−2) for 5 min
图3. (a) PBS、AuNPs/PAM/Ti3C2水凝胶和AuNPs/PAM/Ti3C2/PRP水凝胶用808 nm、0.4 W∙cm−2的激光照射8 min的升温效应。(b) AuNPs/PAM/Ti3C2/PRP水凝胶经808 nm、不同功率(0.25、0.4、0.75、1 W∙cm−2)的激光照射8 min的升温效应
3.4. AuNPs/PAM/Ti3C2/PRP水凝胶的自愈性评价
观察激光器照射后的水凝胶,发现拼接后的水凝胶不发生脱落分离。水凝胶自愈的机理为金纳米颗粒的光热转化性使水凝胶内部的金硫(RS-Au)动态配位键发生动态交换,从而重新交联起聚合物链,最终达到自修复的目的(图4)。
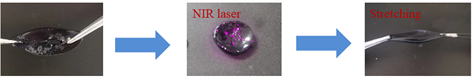
Figure 4. Self-healing procedure AuNPs/PAM/Ti3C2/PRP hydrogel under laser irradiation
图4. 破裂的AuNPs/PAM/Ti3C2/PRP水凝胶在激光照射下愈合效果图
3.5. AuNPs/PAM/Ti3C2/PRP水凝胶的生物相容性研究
理想的伤口敷料必须具有良好的生物相容性,本实验中通过CCK8实验和活/死染色实验来评估水凝胶的生物相容性。如图5(a)所示,CCK8实验表明,AuNPs/PAM/Ti3C2水凝胶组和AuNPs/PAM/Ti3C2/PRP水凝胶组的细胞存活率均高于100%,且AuNPs/PAM/Ti3C2/PRP水凝胶组细胞活力明显高于AuNPs/PAM/Ti3C2水凝胶组。活/死染色图片显示(图5(b)),所有的水凝胶组大多数细胞都是活的(绿色),死亡的细胞占比很少(红色)。不仅如此,可以看出AuNPs/PAM/Ti3C2/PRP水凝胶组绿色荧光明显增强,证明其活细胞数显著增加。这一结果和CCK8实验一致,说明AuNPs/PAM/Ti3C2/PRP水凝胶具有良好的生物相容性且能够促进细胞增殖能力。
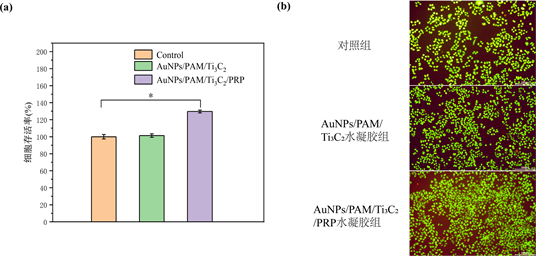
Figure 5. (a) The cell survival rate after coincubation with hydrogel extract; (b) Fluorescence microscopy images of live (green) and dead (red) cells after Calcein-AM/PI double staining for each treatment group
图5. (a) 细胞与水凝胶浸提液共培养后的存活率;(b) 各处理组Calcein-AM/PI双染后活细胞(绿色)和死亡细胞(红色)荧光显微镜图像
4. 结论
综上所述,本研究成功制备了具有优异粘附性、自愈性、拉伸性和光热转化性能的AuNPs/PAM/Ti3C2/PRP智能纳米水凝胶敷料,其表现出极低的细胞毒性和明显的促进细胞增殖特性。后续我们打算开展动物实验进行进一步研究。总而言之,AuNPs/PAM/Ti3C2/PRP智能纳米水凝胶敷料在新型皮肤伤口敷料领域具有广阔的应用前景。
基金项目
山东省自然科学基金创新与发展基金资助项目(ZR2022LSW024)。
参考文献
NOTES
*通讯作者。