摘要: 与Luminal型乳腺癌、人类表皮生长因子受体2 (HER2) (+)乳腺癌相比,三阴性乳腺癌(Triple-Negative Breast Cancer, TNBC)缺乏靶向治疗的特异性靶点,具有生物学侵袭性、复发转移风险高、生存期较短等特点。目的:评估肿瘤浸润淋巴细胞(Tumor Infiltrating-Lymphocytes, TILs)与表皮生长因子受体(EGFR)表达的预后价值,并确定它们与TNBC的临床病理参数之间的关系。材料与方法:收集2010年1月至2015年12月共计70例于青岛大学附属医院接受手术治疗的、有病理报告和临床资料完整的TNBC患者。评估手术标本中TILs比例,并分为高比例(TILs ≥ 40%,n = 28)和低比例(TILs < 40%,n = 42) 2组。免疫组化检测ER、PR、HER2和EGFR的表达,评估EGFR表达情况,并将其分为强阳性组(EGFR ≥ 50%,n = 10)和非强阳性组(EGFR < 50%,n = 60)。评估TILs比例和EGFR表达对预后的影响。结果:TILs低比例组中位无病生存期(DFS) 55.5个月,TILs高比例组97个月,两组比较p = 0.059;TILs低比例组中位总生存期(OS) 69.5个月,高比例组97个月,p = 0.084。EGFR非强阳性组,低比例TILs (TILs < 40%, n = 25)中位DFS和OS分别为24个月和36个月,高比例TILs (TILs ≥ 40%, n = 35)中位DFS和OS均为96个月,不同TILs比例组之间DFS (p = 0.035)和OS (p = 0.048)具有统计学显著性差异;EGFR强阳性组,低比例TILs (TILs < 40%, n = 7)中位DFS和OS均为98个月,高比例TILs (TILs ≥ 40%, n = 3)中位DFS和OS均为94个月(p = 0.513和p = 0.882)。结论:不同TILs比例三阴性乳腺癌患者治疗后DFS和OS差别无统计学显著性。EGFR非强阳性的TNBC患者,TILs比例越高、术后DFS和OS均越长。
Abstract:
Compared with Luminal breast cancer and HER2 (+) breast cancer, triple-negative breast cancer (TNBC) lacks specific targets for targeted therapy, and is characterized by biological invasions, high risk of recurrence and metastasis, and short survival. Objective: To evaluate the prognostic value of tumor infiltrating-lymphocytes (TILs) and epidermal growth factor receptor (EGFR) expression, and to determine their relationship with clinicopathological parameters of TNBC. Materials and Methods: 70 TNBC patients with complete pathological reports and clinical data between January 2010 to December 2015 in Affiliated Hospital of Qingdao University were selected. TILs proportions in sur-gical specimens were assessed and divided into high (TILs ≥ 40%, n = 28) and low groups (TILs < 40%, n = 42). The expression of ER, PR, HER2 and EGFR were detected by immunohistochemistry. EGFR expression was evaluated and divided into strongly positive group (EGFR ≥ 50%, n = 10) and non-strongly positive group (EGFR < 50%, n = 60). The effect of TILs ratio and EGFR expression on prognosis was evaluated. Results: Median disease-free survival (DFS) and total survival (OS) were 55.5 and 69.5 months, respectively, in the low-proportion TILs group, and both of them were 97 months in the high-proportion TILs group. There were no statistically significant differences in DFS (p = 0.059) and OS (p = 0.084) in different TILs proportion groups. In EGFR non-strongly positive group, median DFS and OS were 24 and 36 months, respectively, in the low-proportion TILs group (TILs < 40%, n = 25). Median DFS and OS were 96 months in the high-proportion TILs group (TILs ≥ 40%, n = 35). There were statistically significant differences in DFS (p = 0.035) and OS (p = 0.048) in different TILs proportion groups. In EGFR positive group, median DFS and OS were 98 months in the low-proportion TILs group (TILs < 40%, n = 7), and median DFS and OS were 94 months in the high-proportion TILs (TILs ≥ 40%, n = 3) (p = 0.513 and p = 0.882). Conclusion: TILs ratio and EGFR expression had no significant effect on post operative DFS and OS in patients with triple negative breast cancer. In TNBC patients without strong EGFR, the higher the proportion of TILs, the longer the postoperative DFS and OS.
1. 引言
世界卫生组织国际癌症研究机构(IARC)发布了2020年全球癌症负担数据,全球乳腺癌新发病例高达226万例,超过肺癌的220万例,乳腺癌取代肺癌,成为全球第一大癌症 [1]。根据经典激素和生长因子受体[包括雌激素受体(ER)、孕激素受体(PR)和人类表皮生长因子受体2 (HER2)]的IHC表达,以及Ki-67表达,将乳腺癌分为4个亚型:Luminal A (ER+和PR+,HER2−,Ki-67 < 14%),Luminal B (ER+和/或PR+,HER2+或HER2−,Ki-67 > 14%),HER2过表达型(ER−,PR−,HER2+)和三阴性乳腺癌 [2]。TNBC的ER、PR及HER2免疫组化染色均为阴性,约占所有乳腺癌的15%~20% [3],与非TNBC相比更容易出现早期复发和预后不良,5年生存率仅有60% [4]。
肿瘤浸润淋巴细胞(Tumor-Infiltrating Lymphocytes, TILs)是存在于肿瘤实质与间质内的免疫细胞,是体内免疫系统对肿瘤局部免疫应答的直接反应,也是肿瘤微环境的重要组成部分。有研究发现,乳腺癌组织内TILs比例与乳腺癌患者的预后相关 [5]。TILs作为乳腺癌预测和预后生物标志物的潜在价值,正在日益受到重视。部分TNBC的肿瘤病灶内存在高密度的淋巴细胞浸润,肿瘤细胞、肿瘤基质和肿瘤免疫微环境(Tumor Immune Microenvironment, TIME)之间存在相互作用,可能对TNBC的临床治疗效果产生显著影响 [6]。
人表皮生长因子受体(Epidermal Growth Factor Receptor, EGFR)家族由四种EGFR组成:EGFR (ErbB1或HER1)、HER2 (ErbB2)、HER3 (ErbB3)、HER4 (ErbB4)。EGFR是一种跨膜糖蛋白,包括:细胞外配体结合区域、跨膜区、细胞内酪氨酸激酶活性(Tyrosine Kinase, TK)区。配体和EGFR胞外区域结合后,诱导TK区域酪氨酸残基的磷酸化、从而诱导产生细胞效应:包括激活下游磷酸肌醇3激酶(Phosphatidylinositol-3-Kinase, PI3K)、c-JunN端激酶(c-JunK)、丝裂原激活蛋白激酶(Mitogen-Activated Protein Kinase, MAPK)信号传导通路,导致细胞增生、迁移和存活(防止凋亡)。经典的小分子EGFR抑制剂,如吉非替尼和奈拉替尼治疗TNBC,患者耐药性强、治疗有效性差。EGFR变体III (EGFR variant III, EGFRvIII)是一个有吸引力的嵌合抗原受体T (Chimeric Antigen Recepter T-cell, CAR-T)细胞治疗靶点,因为其表达具有肿瘤抑制性,从而降低了CAR-T识别正常组织抗原。临床研究证实,EGFRvIII特异性CAR-T细胞可以抑制免疫衰竭、改善神经胶质细胞瘤的疗效。临床上也正在研究将检查点阻断抗体和EGFR-CAR-T联合治疗的效果,后者逆转肿瘤免疫抑制性微环境 [7]。
在本研究中,我们旨在评估TILs比例和肿瘤细胞EGFR表达及其预后价值,并确定它们与TNBC的临床病理参数之间的关系,为临床治疗和研究提供分子病理学数据。
2. 材料与方法
1) 临床资料:
收集2010年1月至2015年12月共计70例于青岛大学附属医院只接受手术治疗的、有病理报告和临床资料完整的TNBC患者,入选标准:1) 手术标本均采用免疫组化(IHC)检测诊断为TNBC;2) 所有患者均以根治性乳房切除术、改良根治性乳房切除术或单纯乳房切除术为主要手术治疗选择。患者年龄为32~80岁,中位年龄为50.5岁。排除标准:1) 临床病理资料不完整;2) 局部切除标本。具体临床参数。见表1。

Table 1. Clinical parameters of TNBC
表1. TNBC的临床参数
2) 病理评估
取每位患者的福尔马林固定和石蜡包埋(FFPE)组织。来自组织块的苏木精–伊红(HE)染色切片由两名经验丰富的乳腺癌病理学家进行复核,详细记录组织学参数(ER、PR、HER2、组织病理类型、分级、TILs比例、EGFR表达等)。根据Scarff-Bloom-Richardson系统评估组织学分级。通过IHC和FISH评估肿瘤的三阴性表型(ER、PR和HER2)。
a) 计算TILs比例
利用苏木精–伊红(H&E)染色方法对手术标本进行染色,在光学显微镜(×100倍)下,计算肿瘤间质TILs的面积占肿瘤总面积的百分比,取平均值定义为TILs比例。具体步骤:1) 低倍镜大体扫视整体肿瘤间质细胞;2) 确定TILs评估区域计数:包括肿瘤边界位置的TILs,不计数瘤外、上皮内、瘤周的三级淋巴结构及大片坏死及纤维化区域的TILs;3) 计算间质TILs比例:间质内TILs的面积占肿瘤总面积的百分比 [8]。
目前,对于TILs的界值并没有统一的定义,AiErken等人将TILs分为三组:低比例组(0%~10%)、中等比例组(11%~40%)和高比例组(41%~100%) [9],Byun等人将TILs分为TILs ≥ 33%和TILs < 33% [10],Leon-Ferr等人将淋巴细胞优势性乳腺癌定义为TILs比例 > 50% [11]。本文将TILs比例 < 40%定义为低比例组(n = 42),TILs比例 ≥ 40%定义为高比例组(n = 28)。三阴性乳腺癌中TILs分布比例。见图1。
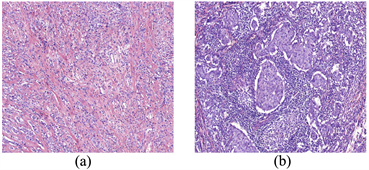
Figure 1. Proportion of TILs in triple-negative breast cancer. (a) TILs < 40%; (b) TILs ≥ 40% (×100)
图1. 三阴性乳腺癌中TILs分布比例。(a) TILs < 40%;(b) TILs ≥ 40% (×100)
b) EGFR评估
将5 μm肿瘤切片从福尔马林固定的石蜡包埋块上切割下来,切片经二甲苯脱蜡,用分级乙醇水化;然后用高压法进行抗原修复;之后去除内源性过氧化物酶活性,然后滴加EGFR抗体(小鼠单克隆IgG EGFR抗体,Roche公司),4℃过夜,再滴加酶标羊抗鼠/兔IgG聚合物,最后,用二氨基联苯胺底物进行染色,切片用苏木精复染;最后,脱水、透明、封片。对于EGFR判读,肿瘤细胞细胞浆、细胞膜、或者胞浆和膜同时染色,指示EGFR阳性染色。综合Morinaga等(2006)、Buckley等(2008)、Harder等(2009)的文献,高倍镜下阳性细胞数量占评估细胞总数的百分比作为定量的标准 [12]:
• 0没有阳性细胞,即阴性;
• 1+阳性细胞数量占比1%~10%,即弱阳性;
• 2+阳性细胞数量占比11%~50%,即阳性;
• 3+阳性细胞数量占比 ≥ 50%,即强阳性;
本研究将EGFR分为强阳性组(n = 10)和非强阳性组(n = 60),即阴性、弱阳性及阳性。见图2。
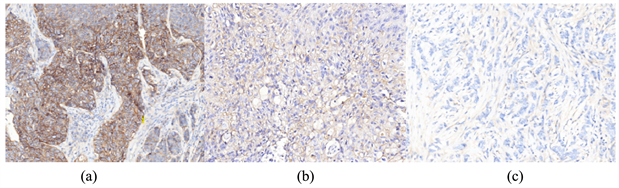
Figure 2. EGFR expression in triple-negative breast cancer. (a) EGFR strongly positive expression; (b) EGFR positive or weakly positive expression; (c) EGFR negative expression
图2. 三阴性乳腺癌中EGFR表达情况。(a) EGFR强阳性表达;(b) EGFR阳性或弱阳性表达;(c) EGFR阴性表达
3) 随访
随访以门诊复查记录及电话访谈形式进行,以获取局部复发或远处转移、治疗后生存状态等预后信息。中位随访时间为81.5个月,完成随访比例47/70,23例患者失访。无病生存期(DFS)和总生存期(OS)被用作生存分析的终点。DFS定义为从首次接受治疗到出现复发转移或失去随访的日期;OS定义为从首次接受治疗到死亡或失去随访的日期。
4) 统计分析
采用SPSS 26.0统计软件(SPSS Inc, Chicago, IL, USA)进行统计分析。采用卡方检验比较组间相关因素。采用log-rank检验和Kaplan-Meier (K-M)曲线评价组间影响因素及生存差异。p < 0.05为差异具有统计学意义。
3. 结果
本研究共纳入70例TNBC患者,分析TILs比例和EGFR表达情况。
1) TILs分组/EGFR表达和临床病理参数之间的关系。TILs比例与组织学类型显著相关,与其它病理学标记物表达情况无明显统计学差异;EGFR蛋白表达与各临床病理参数均无显著统计学差异。见表2。

Table 2. Relationship between TILs grouping/EGFR expression and clinicopathological parameters
表2. TILs分组/EGFR表达和临床病理参数之间的关系
注:pN*:4例Nx排除。
2) TILs与预后的关系。
a) TILs比例对总体生存期(OS)的影响。TILs < 40%,中位生存期为69.5个月;TILs ≥ 40%,中位生存期97个月,p = 0.084。见图3。

Figure 3. Influence of TILs ratio on OS
图3. TILs不同比例对OS的影响
b) TILs比例对无病生存期(DFS)的影响。TILs < 40%,中位生存期为55.5个月;TILs ≥ 40%,中位生存期97个月,p = 0.059。见图4。
3) EGFR表达与TILs比例对预后的影响
a) EGFR表达与TILs比例对总体生存期(OS)的影响。EGFR非强阳性组,TILs < 40%组中位生存期为36个月,TILs ≥ 40%组中位生存期为96个月(p = 0.048),有统计学差异;EGFR强阳性组,TILs < 40%组中位生存期为98个月,TILs ≥ 40%组中位生存期为94个月(p = 0.882)。见图5。
b) EGFR表达与TILs比例对无病生存期(DFS)的影响。EGFR非强阳性组,TILs < 40%组中位生存期为24个月,TILs ≥ 40%组中位生存期为96个月(p = 0.035),有统计学显著性差异;EGFR强阳性组,TILs < 40%组中位生存期为98个月,TILs ≥ 40%组中位生存期为94个月(p = 0.992)。见图6。
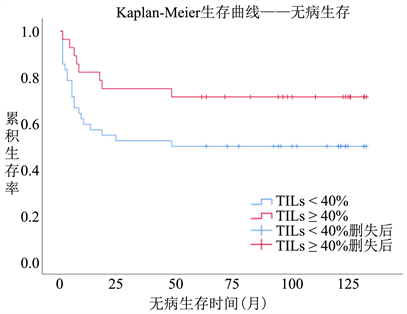
Figure 4. Influence of TILs ratio on DFS
图4. TILs不同比例对DFS的影响


Figure 5. Influence of TILs ratio and EGFR expression on OS
图5. EGFR表达与TILs比例对OS的影响

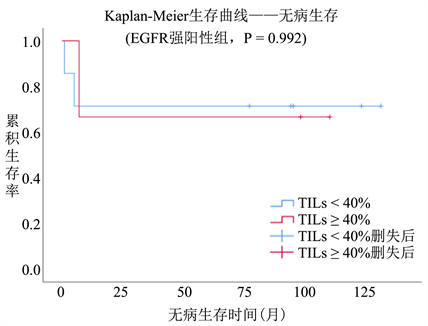
Figure 6. Influence of TILs ratio and EGFR expression on DFS
图6. EGFR表达与TILs比例对DFS的影响
4. 讨论
1) 基底样型乳腺癌主要为ER、PR和HER2阴性的三阴性乳腺癌(TNBC),以EGFR、CK5/6、CK14和CK17表达阳性为特征。70%~80%的TNBC为基底样型 [13]。O’Meara T等人发现,TNBC免疫调节(Mmunomodulatory, IM)亚型TILs比例较高,且以CD8表达阳性淋巴细胞为主,组织学类型以髓样癌(伴有髓样特征的乳腺癌)为主 [14]。笔者分析的70例TNBC中,基底细胞样型52例(74%),其中22例(42%)TILs ≥ 40%;导管型15例,3例(20%) TILs ≥ 40%;其他类型(鳞状细胞癌+髓样癌)共计3例,均为TILs < 40% (p = 0.029),基底样亚型TNBC TILs比例更高,和O’MearaT等的发现有所不同。
2) TILs可以预测新辅助化疗的病理完全缓解率(pathological Complete Response, pCR)。GeparSixto试验,使用蒽环类 + 紫杉类药物 ± 铂类进行化疗,TILs预测TNBC pCR的结果:TILs ≥ 60%组(n = 142) pCR为59.9%、TILs < 60%组(n = 438)只有33.8% (p < 0.001) [15]。荟萃分析表明,治疗前活检组织中TILs数量越多、新辅助化疗的pCR比例越高(OR = 3.93,95% CI 3.26~4.73) [16]。肿瘤细胞坏死释放出肿瘤相关抗原,触发针对肿瘤细胞的免疫应答反应,TILs比例越高,免疫应答越明显。TILs比例越高的TNBC,化疗能诱导更强烈的免疫应答反应,导致肿瘤细胞的坏死更为明显,治疗疗效越好、患者生存期越长。因此,组织病理学TILs计数,可以作为TNBC综合治疗疗效的独立预测和预后指标,高TILs计数患者受益于术前化疗。本组70例患者只有1例接受了术前化疗,化疗前也没有对活检标本进行TILs计数,值得在以后的工作中进行改进。
TILs可以预测TNBC综合治疗后的生存效果。BIG02-98试验中,共有256例TNBC患者接受了基于蒽环类药物的化疗,分析表明TILs和化疗疗效显著相关:TILs的百分数每增加10%,乳腺癌复发和转移风险分别降低17%和15% [17]。对III期临床试验ECOG-21971和ECOG-1199的结果进行回顾性分析,也得出了类似的结论:TILs每增加10%,复发风险下降14% (p = 0.02)、转移风险下降18% (p = 0.04)、死亡风险下降19% (p = 0.01) [18]。笔者以40%为标准将70例TNBC进行分组,TILs高比例组(≥40%,n = 28)治疗后中位无病生存时间(97个月)要明显优于TILs低比例组(<40%,n = 42) (55.5个月) (p = 0.059)。TILs高比例组(≥40%,n = 28)治疗后中位总体生存时间(97个月)要优于TILs低比例组(<40%,n = 42)(69.5个月) (p = 0.084),虽然差异没有达到统计学显著性,但是较长生存趋势是比较明显的。由于样本数量较小(n = 70),无法按照10%的阶梯进行分析,计划以后补充数据后再进行验证。
3) TNBC中EGFR的突变频率,多数报道在0%~11.4%之间,随种族、检测方法不同而异,类似于NSCLC EGFR在亚洲人(20%~50%)中的突变频率高于西方人(15%~20%) [19]。日本、欧洲、澳大利亚TNBC患者没有EGFR基因的激活突变,韩国TNBC患者EGFR外显子19、外显子21的激活突变频率1%~2%,中国人的突变频率高达10%。除了EGFR激活突变外,在0%至24%和7%至64%的TNBC中,分别出现了EGFR扩增和高多样体(polysomy) [20]。Park等人报道EGFR过度表达(2+或3+)与TNBC的低分期显著相关,但与其他临床病理变量或临床结果无关,也不能预测患者的生存率 [21]。本组结果与之类似:EGFR过度表达比例14.3% (10例/70例),EGFR表达与否对TNBC患者OS (p = 0.882)和DFS (p = 0.992)影响有限。文献报道,在乳腺癌中未发现EGFR过度表达与EGFR基因突变之间存在相关性 [22]。笔者只使用IHC检查EGFR蛋白质表达的情况,没有使用FISH检查基因扩增的情况,因此在评估是否存在EGFR过度表达上存在一定的缺陷。
在细胞接触时,EGFR可以通过胞啃作用,从一个细胞转移到另一个细胞,因此EGFR能够从癌细胞转移到TILs,导致TNBC细胞上EGFR水平下降,TILs比例越高,癌细胞EGFR表达越低;EGFR下调还可诱导PD-L1在癌细胞上的表达降低,降低PD-L1/PD-1通路对T细胞的免疫抑制作用,从而提高免疫抑制剂在TNBC中的疗效 [23]。我们的研究结果为此提供了佐证:EGFR非强阳性表达的患者(n = 60),TILs ≥ 40%组(n = 25)治疗后中位无病生存时间(96个月)和总生存时间(96个月)均显著优于TIL < 40%组(n = 35)的中位无病生存时间(24个月)和总生存时间(36个月) (p = 0.035和p = 0.048)。对EFGR非强阳性的、高TILs计数的TNBC患者,值得进行化疗联合免疫检测点治疗抑制剂的新辅助治疗的临床试验。邵志敏等人对中国465例原发性TNBC的相关资料进行了全面分析,提出了TNBC的复旦分子分型:雄激素受体型(Luminal Androgenreceptor, LAR)、免疫调节型(Immunomodulatory, IM)、基底样免疫抑制型(Basal-Like Immunosuppressed, BLIS)和间充质型(Mesenchymal, MES) [24]。随后,进一步验证了基于复旦分子分型的靶向药物选择是TNBC精准治疗的重要依据 [25]。笔者认为,EGFR和TILs是TNBC治疗预后相关重要病理学参数,针对EGFR非强阳性表达的患者设计化疗 + 免疫治疗的方案、针对EGFR过度表达设计CAR-EGFR细胞治疗的方案,将为TNBC治疗带来新的飞跃。
NOTES
*通讯作者Email: weizmqdfy@qdu.edu.cn