摘要: 目的:探讨粪菌移植技术对脓毒症小鼠肠粘膜屏障的影响。方法:按随机数字表法将75只雄性ICR小鼠分为3组:假手术组、脓毒症组和脓毒症 + 粪菌移植组,每组25只。采用盲肠结扎穿孔方法制作脓毒症小鼠模型。各组取10只小鼠观察7 d存活率;剩余小鼠分别于制模后12、24、48 h心脏取血后各处死5只,测定血清IL-6、IL-10、TNF-α和高迁移率族蛋白B1(HMGB1)水平;并在光镜下观察脓毒症小鼠小肠组织病理学改变并进行评分。结果:粪菌移植治疗组小鼠7 d存活率较脓毒症组小鼠组改善(P < 0.05);与假手术组比较,脓毒症组造模后12、24及48 h血清IL-6、IL-10、TNF-α、HMGB1均有差异(P < 0.05);与脓毒症组相比,在造模后12、24及48 h粪菌治疗干预后,粪菌移植组小鼠的血清TNF-α、IL-6、IL-10及HMGB1均明显下降(P < 0.05),但仍高于假手术组(P < 0.05);光镜下小肠组织病理学改变,与假手术组相比,在造模后12、24及48 h,脓毒症组小鼠肠组织损伤评分明显升高(P < 0.05);与脓毒症组相比,造模后12 h粪菌移植组小鼠肠组织损伤评分无显著差异(P > 0.05),而24、48 h的时间点粪菌移植组小鼠肠组织损伤评分偏低(P < 0.05)。结论:粪菌移植治疗能够降低严重脓毒症小鼠炎症反应并减轻由其引起的肠组织损伤,从而改善脓毒症进程,提高存活率。
Abstract:
Objective: To investigate the effects of fecal microbiota transplantation on serum inflammatory fac-tors and intestinal injury in mice with sepsis. Methods: A total of 75 male C57BL/6 mice were ran-domly and equally divided into three groups: sham operation, sepsis, and sepsis + fecal microbiota transplantation. Severe sepsis model was induced by cecal ligation and puncture in mice. Ten mice in each group were monitored for the 7-d survival rate, and the remaining were killed 12, 24, and 48 h after the model was established. The levels of IL-6, IL-10, and high mobility group protein B1 (HMGB1) were measured. Results: The 7-day survival rate of severe sepsis mice was 0, and the 7-day survival rate of fecal bacteria transplantation group was increased to 50%; the difference was statistically significant compared to the model group (P < 0.05). Compared to the sham operation group, the sepsis group had higher serum creatinine levels at 12, 24, and 48 h after modeling, and the levels of TNF-α, IL-6, IL-10, and HMGB1 were significantly increased (P < 0.05). Compared to the sepsis group, the levels of serum TNF-a, IL-6, IL-10, and HMGB1 in the fecal bacteria transplantation group were significantly decreased (P < 0.05) after 12, 24, and 48 h of fecal bacteria treatment (P < 0.05), but still higher than those in the sham operation group (P < 0.05). Compared to the sepsis group, the intestinal tissue injury score of the fecal bacteria transplantation group did not show a significant difference at 12 h after modeling (P > 0.05), but the intestinal tissue injury score of the fecal bacteria transplantation group was lower at 24 and 48 h after modeling (P < 0.05). Conclusion: Fecal microbiota transplantation decreases the inflammatory response and intestinal tissue dam-age in severe sepsis mice and improves the survival rate.
1. 引言
脓毒症(Sepsis)是由感染引起的急危重症,重度脓毒症可继发严重的多脏器功能衰竭和脓毒性休克,其病死率可达50%以上 [1]。1986年Carrico等 [2] 提出“胃肠道是MODS的始动器官”的著名论点。肠道菌群在脓毒症的发生发展中起关键作用,其主要与脓毒症时血流动力学改变、炎性细胞因子的产生、氧化应激反应等对肠道微生态、肠道黏膜屏障等损伤有关 [3] [4]。随着肠道菌群的研究进展,粪菌移植(Fecal microbiota transplantation, FMT)受到青睐,肠道共生菌对抵御病原体入侵、提供生物屏障及调节免疫等方面具有重要作用 [5]。研究报道粪菌移植通过重建肠道菌群,对艰难梭菌感染引起的多脏器功能衰竭的患者具有一定疗效 [6] [7]。本研究拟通过观察脓毒症小鼠接受粪菌移植治疗后血清炎性因子水平和肠组织的病理变化,进而探讨粪菌移植对严重脓毒症小鼠的保护作用及机制。
2. 材料与方法
2.1. 实验动物及分组
成年雄性C57BL/6小鼠6~8周龄,体重20~25 g,由山东大学医学科学院实验动物中心(济南)饲养并提供,控制动物房室温于22℃~24℃,相对湿度约50%,自然昼夜光线照明,动物可自由进食水,常规饲养1周使其适应饲养环境后用于实验研究。按照随机数字表法将实验动物分为三组(n = 75):假手术组、脓毒症组和脓毒症 + 粪菌移植组。本实验中以及后续实验中所涉及实验步骤及过程均经泰安市中心医院动物实验管理委员会批准。
2.2. 模型制备及处理
2.2.1. 脓毒症小鼠模型建立
采用盲肠结扎穿孔术(cecal ligation and puncture, CLP) [8] 制备脓毒症小鼠模型,10%水合氯醛30 mg/kg腹腔注射麻醉小鼠,腹部皮肤消毒,沿腹中线切口,从距离盲肠盲端约1/3处结扎盲肠(注意勿结扎回盲瓣及盲肠系膜血管)。以20号无菌注射器针头于盲肠末端贯通穿孔,挤出少量肠内容物,还纳腹腔并逐层缝合腹壁。对照组只进行腹腔探查术,不进行盲肠结扎和穿孔。小鼠术后经颈部皮下注射生理盐水50 ml/kg进行液体复苏。
2.2.2. 粪便菌群制备和移植 [9]
按摩刺激对照组小鼠腹部排便,收集新鲜粪便,置于消毒的离心管中,将收集的粪便称重,加入37℃无菌生理盐水混匀,双层无菌纱布过滤掉残渣,6000 rpm,4℃离心5分钟,沉淀颗粒物,取上清液制成400 mg/ml浓度的FMT混悬液,每次FMT后留存500 uL菌液−80℃存放用于菌群分析。参考人体粪菌移植标准 [10],每次移植的粪菌相当于小鼠自身体重的1/500的粪便量。进行FMT干预:用一个圆尖硅胶管将制备好的FMT混悬液注射入结肠内,每天1次,持续3天。硅胶管插入小鼠结肠中约1~3.5厘米。注射完后,将小鼠头朝下垂直悬吊1分钟以减少损失 [11]。
制模后每组各取10只于标准条件下饲养,连续观察7 d并记录存活率,观察期间及时移除死亡动物尸体,以免对饲养环境造成污染。余各组15只小鼠于造模后12 h、24 h及48 h各处死5只备检。
2.3. 检测指标及方法
2.3.1. 炎性因子检测
于造模后12 h、24 h及48 h麻醉小鼠,沿原切口切开腹壁并充分暴露,在距回盲瓣2 cm处取回肠组织并制备组织匀浆。采取酶联免疫吸附试验(ELISA)测定肠道组织中促炎性细胞因子肿瘤坏死因子-α (Tumour necrosis factor-α, TNF-α)、白细胞介素-6 (Interleukin-6, IL-6)、和高迁移率族蛋白1 (High mobility group box-1, HMGB1)以及抗炎性细胞因子白细胞介素-10 (Interleukin-10, IL-10)的水平评价肠道组织的炎症反应情况。
2.3.2. 光镜下观察小肠组织病理学改变
于造模后12 h、24 h及48 h麻醉小鼠,沿原切口切开腹壁并充分暴露,在距回盲瓣2 cm处取回肠组织备用。组织用10%的福尔马林固定后,依次经梯度乙醇脱水、石蜡包埋、组织切片、二甲苯脱蜡后HE染色。光镜下观察结肠组织的病理变化,并进行肠组织损伤评分 [12],以0~5分分别代表了不同程度的肠道损伤。具体评分标准为:0分为正常肠粘膜绒毛结构;1分为肠黏膜绒毛顶端出现上皮下Gruenhagen’s间隙(通常发生在绒毛的顶端),常常伴随毛细血管轻度扩张充血;2分为肠上皮下间隙的中度扩张和粘膜层与固有层的分离和轻度抬高;3分为大片肠黏膜上皮抬高,部分绒毛顶端脱落;4分为肠绒毛及固有层脱落,扩张的毛细血管裸露在外;5分为固有层蜕变或被消化,伴有出血或溃疡形成。
2.4. 统计学分析
统计学分析:采用SPSS18.0统计软件进行数据分析。采用Fisher确切概率法进行组间比较。计量资料以均数 ± 标准差(x ± s)表示,组间比较采用单因素方差分析,两两比较采用LSD检验,采用Kaplan-Meier生存分析方法。P < 0.05表示差异有统计学意义。
3. 结果
1) 粪菌移植治疗后小鼠体重变化趋势,可缓解小鼠体重下降(图1);粪菌移植治疗对脓毒症小鼠存活率的影响(图2):粪菌移植治疗显著提高了脓毒症小鼠的存活率(P < 0.05)。
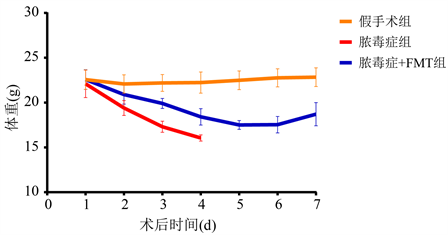
Figure 1. The weight change levels in each group of mice
图1. 各组小鼠体重变化水平
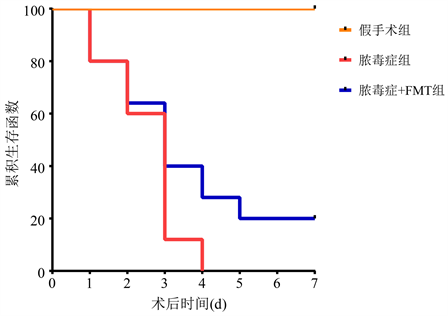
Figure 2. The 7-days survival rate of groups
图2. 各组小鼠7天生存分析
2) 粪菌移植治疗对严重脓毒症小鼠血清炎性因子的影响(表1):与假手术组相比,在造模后12、24及48 h,脓毒症组小鼠的血清TNF-α、IL-6、IL-10及HMGB1均明显升高(P < 0.05);与脓毒症组相比,在造模后12、24及48 h粪菌治疗干预后,粪菌移植组小鼠的血清TNF-α、IL-6、IL-10及HMGB1均明显下降(P < 0.05),但仍高于假手术组(P < 0.05)。光镜下小肠组织病理学改变(图3),与假手术组相比,在造模后12、24及48 h,脓毒症组小鼠肠组织损伤评分明显升高(P < 0.05);与脓毒症组相比,造模后12 h粪菌移植组小鼠肠组织损伤评分无显著差异(P > 0.05),而24、48 h的时间点粪菌移植组小鼠肠组织损伤评分偏低(P < 0.05)。

Table 1. Intestinal inflammatory cytokines level of the three group at 12, 24 and 48 h after CLP operation; HE staining of intestinal tissue from the three group at 12, 24 and 48 h after CLP operation (
)
表1. 粪菌移植治疗对严重脓毒症小鼠不同时间点血清炎性因子及肠组织病理学评分(
)
*:P < 0.05,与假手术组比较;#:P < 0.05,与脓毒症组比较。

Figure 3. HE staining of intestinal tissue from the three group at 12, 24 and 48 h after CLP operation
图3. 光镜下观察术后12 h、24 h和48 h各组小鼠小肠组织病理学改变
4. 讨论
本研究主要是通过经典的盲肠结扎穿孔诱导重度脓毒症 [8],通过造成肠腔穿孔至粪便进入腹腔,进而引起肠道菌群的混合感染诱导重度脓毒症。此外,盲肠结扎导致肠供血中断,肠组织缺血坏死,释放大量炎性因子对诱发脓毒症起着关键作用 [13]。本研究脓毒症模型小鼠的7 d存活率为0,血清炎性因子TNF-α、IL-6及HMGB1较假手术组明显升高,且肠组织病理学评分显著增高,证明重症脓毒症小鼠模型制备成功。
粪菌移植(FMT) [14] [15] 是指通过从正常粪便中分离的多种微生物及其代谢产物,通过一定途径(鼻胃管、鼻十二指肠管、胃镜、结肠镜或直肠导管灌肠等)输入到患者肠道内,用以重新建立肠道菌群的多样性,修复肠粘膜屏障功能,调节免疫功能,对疾病的发生、发展具有一定的治疗作用。
临床研究发现脓毒症患者中肠道菌群存在高度特异性,其主要包括细菌菌数的多样性显著下降,微生物的生理功能丢失及单一菌群的过度生长 [16]。肠道微生物群的丰富性和平衡性对维持肠道屏障功能具有重要作用 [17]。肠道是脓毒症的始动器官,肠道屏障功能障碍在SIRS-Sepsis-MODS的连续发展过程中具有重要的作用,肠屏障功能改变,通透性增加,肠道细菌和内毒素移位,导致大量炎性介质和细胞因子释放,从而可加剧屏障功能的改变和影响各器官功能,最终导致MODS。本研究中我们观察到,脓毒症小鼠的小肠组织病理学评分明显升高,而接受了粪菌移植治疗的小鼠肠组织损伤明显减轻,但组织病理学评分虽仍高于假手术组。此外粪菌移植治疗组的小鼠存活率明显提高,但仍低于假手术组。因此,粪菌移植治疗可能通过重新建立肠道菌群的多样性、修复肠粘膜屏障功能,从而减少肠上皮细胞凋亡并减轻肠组织损伤,对改善脓毒症进程,提高存活率有一定作用。
脓毒症是有感染诱发的,免疫系统对入侵的感染性微生物的不受控制的过度反应,其特征是促炎介质如IL-6、TNF-α和HMGB1的大量产生可能损害器官功能,导致不同器官的异常凋亡,导致多器官功能障碍综合征和死亡 [18]。其中,HMGB1是脓毒症发展过程中的一种重要晚期炎性介质。此外IL-10具有抑制炎症反应、拮抗炎性介质的作用,能够下调促炎因子TNF-α和IL-6的含量 [19]。本研究中我们观察到,严重脓毒症组小鼠TNF-α、IL-6、IL-10和HMGB1含量于制模后明显升高;粪菌移植治疗组脓毒症小鼠血清TNF-α、IL-6和HMGB1含量均明显下降,但仍高于假手术组。因此,粪菌移植能够提高严重脓毒症小鼠血清抗炎因子IL-10的含量,降低血清TNF-α、IL-6和HMGB1的含量,从而下调全身炎症反应,对改善脓毒症的进程具有一定的作用。
5. 结论
综上所述,本研究证实粪菌移植能够明显提高严重脓毒症小鼠的存活率,改善肠组织病理特征,减轻炎性因子的释放。为其应用于临床脓毒症患者的治疗提供了理论依据。但在我们的研究中,并未能解释该结果的具体机制,我们考虑可能与肠道菌群的重新建立有关,需要进一步进行实验阐明。
基金项目
泰安市科学技术发展计划(项目编号:2018NS0212)。
NOTES
*通讯作者。