摘要:
目的:回顾性分析1例马蹄肾患儿合并输尿管畸形,异位输尿管的临床资料,并进行相关文献回顾,提高临床上对该疾病的认知。方法:1个4岁的男孩因为反复尿床于当地行B超检查提示肾脏发育异常伴输尿管异常。于我院行体格检查与实验室检查未见异常。行CTU提示:左侧输尿管畸形扩张,右侧输尿管扩张。双侧肾盂肾盏扩张。行于全麻下行双侧输尿管再植术 + 输尿管残端切除术 + 剖腹探查术。结论:马蹄肾常合并泌尿系统畸形并不少见,但该病例合并左侧输尿管畸形,右侧巨输尿管,膀胱内异位输尿管,属实少见,特进行报道,同时阐述下对于膀胱内异位的盲端输尿管如何进行判断处理。
Abstract:
Background: Horseshoe kidneys are mostly asymptomatic, but some patients often have other urogenital, gastrointestinal, cardiopulmonary, skeletal, or chromosomal abnormalities. We describe a 4-year-old boy with horseshoe kidney with left ureter “Y” deformity, bilateral giant ureter, ureteral ectopic and how to treat it and how to treat the ectopic blind end of the ureter in the bladder. Case presentation: A 4-year-old boy was admitted to a local hospital for frequent, dirty and interrupted urination and the B-ultrasound showed renal dysplasia with ureteral abnormalities. In our hospital, Physical examination and laboratory examination showed no abnormality. CTU suggested: left ureter malformation and dilatation, right ureter ectasia, expansion of bilateral renal pelvis and calyces, horseshoe kidney. The child underwent bilateral ureteral replantation under general anesthesia/ureteral stump excision. After a year of follow-up, a clinical examination and imaging findings were unremarkable. Conclusions: It is not uncommon for horseshoe kidneys to be associated with urinary malformation, but this case was associated with left ureter “Y” deformity, bilateral giant ureter, ureteral ectopic. This kind of case is true rare. So we carry on a report especially. We also describe the identification and management of ectopic blind ureters in the bladder.
1. 引言
单纯的马蹄肾大多没有症状,但部分患者常合并有其他泌尿生殖、胃肠道、心肺、骨骼或染色体异常。我们阐述一个4岁的男孩马蹄肾患儿合并左侧输尿管“Y”畸形,双侧巨输尿管,膀胱内输尿管异位及其如何进行治疗。
2. 资料与方法
2.1. 一般资料
患儿,男,4岁。因“B超发现双侧肾盂积水半月”入院。患儿因反复尿床于当地行B超检查示肾脏发育异常伴输尿管异常。体检:体温37.4℃,脉搏90次/分,呼吸23次/分,体重16 kg,血压123/72 mmHg。患者一般状况可,神志清,精神可,皮肤无黄染,浅表淋巴结无肿大,头颈四肢无畸形,甲状腺无肿大,胸廓对称,心肺听诊正常。专科查体:腹部平软,未见胃肠型及蠕动波,腹肌柔软,肝脾肋下未触及,全腹无压痛反跳痛,肾区无叩痛,未触及包块,无压痛反跳痛。实验室检查:白细胞9.05 × 109/L;淋巴细胞百分比24,中性粒细胞百分比65.7;红细胞3.49 × 1012/L;血红蛋白90 g/L;血小板299 × 109/L (参考值:白细胞:5~12 × 109/L,淋巴细胞百分比:40%~70%,中性粒细胞百分比:25%~55%,红细胞:3.75~5.5 × 1012/L,血红蛋白:110~145 g/L,血小板:125~350 × 109/L)。尿常规:白细胞(−),红细胞(−),蛋白(−),辅助检查:(1) B超示双肾畸形,双肾下极于腹主动脉及双侧髂血管前方相连。双肾集合系统分离扩张,输尿管扩张,右侧内径较宽处1.5 cm,左侧内径较宽处1.7 cm,提示:双肾畸形,马蹄肾;双肾积水,双输尿管扩张。(2) 泌尿系统CT造影:双肾体积明显增大、融合,位置下移,实质变薄。双侧肾盂、肾盏明显扩张。右侧输尿管中上段增粗迂曲,其下段显示较细。左侧上段示双输尿管走行迂曲、扩张并汇合成一条输尿管(图1,图2)。入院诊断为肾盂积水,双侧;泌尿系统畸形。
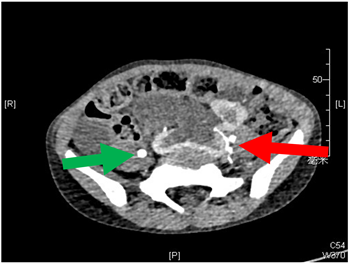
Figure 1. The green arrow is the dilated ureter on the right and the red arrow is the two malformed ureters on the upper left
图1. 绿色剪头为右侧输尿管,红色箭头为左侧输尿管
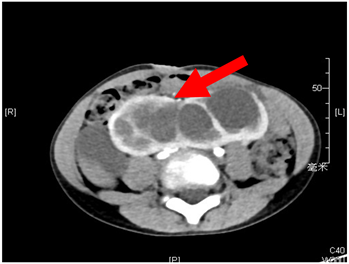
Figure 2. The red arrows represent the fused horseshoe kidney on CT
图2. 马蹄肾
2.2. 手术方法
于全麻下行双侧输尿管再植术 + 输尿管残端切除术 + 剖腹探查术。术中见,左侧重复输尿管在局左侧输尿管上方约3 cm处呈“Y”形于近端汇合成一根进入膀胱(图3)。右侧输尿管下端狭窄,上端扩张。切开膀胱前壁,于左右输尿管口分别置入导尿管,其中左侧插入困难,沿着左侧输尿管开口环形切开膀胱粘膜,分离输尿管末端,逆行解剖输尿管远端,可见输尿管末端狭窄约1 mm,上方输尿管扩张约3 cm,自左输尿管切口向对侧输尿管开口外上方作粘膜下隧道,长约5 cm,于上方做切口,切除狭窄的左侧输尿管,将左侧扩张的经隧道穿出至新开口处,将扩张的输尿管全层与膀胱粘膜5-0可吸收缝线缝合固定,同时缝合原开口处粘膜,放置输尿管支架并固定支架管。右侧输尿管切除近端狭窄部分,同样方式将右侧输尿管再植。继续探查膀胱,发现其中一根多余输尿管,结扎多余输尿管,注入亚甲蓝约5 ml,确认为盲端输尿管后给予切除(图4)。

Figure 3. The black line of the “Y” shape indicates the left “Y” shape of the ureter
图3. 黑色线条为为左侧“Y”形输尿管

Figure 4. The red arrow is the free ureter inside the bladder, the green arrow is the left ureter, and the black arrow is the right ureter
图4. 绿色箭头为左侧输尿管,黑色箭头为右侧输尿管,红色箭头为膀胱内输尿管
3. 讨论
马蹄肾(horseshoe kidney, HSK)是最常见的融合肾畸形,发病率约为1:400,常见于男性,男女的发病率约为2:1 [1] [2],有些学者认为马蹄肾的发生是由于在肾脏发育过程中,胚胎时期肾脏分离异常以及十二指肠下动脉的阻碍,肾脏上升所致 [3]。大部分马蹄肾是在检查中偶然发现的 [4],单纯的马蹄肾大多没有症状,但是也有学者发现超过1/3的马蹄肾患者合并有其他泌尿生殖、胃肠道、心肺、骨骼或染色体异常 [5] [6] [7] [8],此时患者常会产生临床症状,这时候就需要进行临床干预。
巨输尿管指由任何原因引起的扩张的输尿管 > 7 mm以上。巨输尿管根据其成因分为:梗阻型;返流型;非梗阻非返流型;梗阻返流型。其治疗适应症方面存在着一些争议,但对于梗阻型,有肾积水,肾功能损害则建议行手术治疗。尤其在儿童阶段病情进展较快,肾功能的损害较为严重,建议及早手术 [9]。
该马蹄肾患儿合并双侧输尿管畸形,左侧输尿管Y形,右侧远端输尿管狭窄,近端扩张,同时膀胱内有一盲端输尿管。其畸形的输尿管导致双侧肾积水,肾盂扩张,如不处理,会进一步损伤肾皮质,损伤肾功能 [10],需手术治疗其畸形、异位输尿管。该患儿患有马蹄肾合并输尿管畸形合并膀胱内异位输尿管,十分罕见,在处理双侧畸形输尿管的同时,还需注意膀胱内的盲端输尿管,将其结扎,切除。对于手术操作来说并不是十分困难,但是困难的是容易忽略掉其膀胱内的游离输尿管,术中术者用膀胱结扎输尿管的远端,向盲端输尿管注射亚甲蓝,判断该输尿管确实为盲端输尿管,对于膀胱内盲端输尿管的判断不失为一种好方法。
对于马蹄肾合并输尿管畸形合并膀胱内异位输尿管的患儿若无症状可行不需治疗,只需定期复查B超、肾功能。我们报道该例患儿,并回顾相关文献,希望能为其他医生提供一些帮助。
该病例报道已经过患者家属同意,并符合伦理要求。
NOTES
*第一作者。
#通讯作者。